Rapunzel Syndrome Accompanied by Transient Intussusception
By Imtiaz S
CASE SUMMARY
A 4-year-old with a history of trichophagia presented to the emergency department with complaints of generalized abdominal pain, nausea, vomiting, and constipation. The abdominal pain had occurred intermittently for 2-3 months and had worsened in recent days. Physical examination revealed generalized abdominal tenderness. Lab findings were normal except for iron deficiency anemia. An abdominal CT scan was performed and subsequent endoscopy revealed a trichobezoar, which was surgically removed.
IMAGING FINDINGS
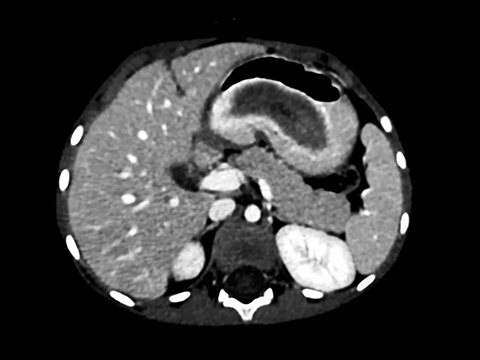
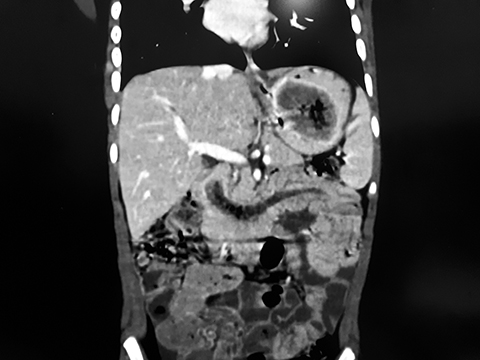
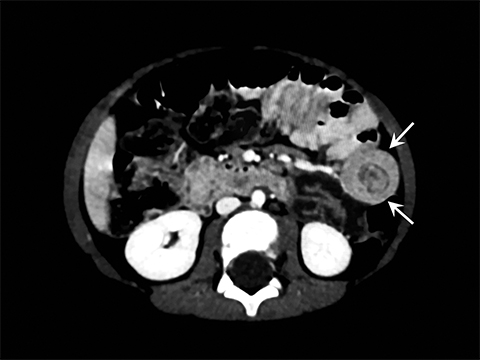
Abdominal CT revealed a large, low-attenuation tubular area with multiple mottled specks of air within the gastric lumen, extending to the duodenum and the proximal jejunal loops (Figures 1, 2) In the proximal jejunum, telescoping of the small bowel loops with incurving of adjacent mesentery was observed; however, the contrast passage into more distal small bowel loops was noted (Figure 3). Findings were consistent with a large trichobezoar causing transient jejuno-jejunal intussusception..
DIAGNOSIS
Rapunzel syndrome
DISCUSSION
Rapunzel syndrome is a rare condition, first described by Vaughan et al in 1968 as a large, gastric trichobezoar that extends from the stomach through the duodenum and jejunum, and potentially to the ileo-cecal junction.1 The term, “Rapunzel syndrome,” derives from a fairy tale, written in 1812 by the Brothers Grimm, telling of the long-haired maiden trapped in a castle who lowered her hair to the ground, permitting her young prince to climb up and rescue her.2 The long tail extending from trichobezoars into the small intestine is said to resemble the maiden’s hair.
Bezoars are masses in the gastrointestinal tract formed by indigestible food or foreign substances; they are classified according to their contents, such as hair (trichobezoar), vegetable or cotton fibers (phytobezoar), dairy products (lactobezoar), drugs (pharmacobezoar), and persimmon fibers (diospyrobezoar).3 Trichobezoars were first described by Baudomont in 1779.4
Approximately 90% of trichobezoars occur in females between 10 and 19 years of age. Half of patients have a psychiatric illness, such as trichophagia and trichotillomania. Thirty percent of patients with trichotillomania develop trichophagia; 1% of those with trichophagia develop trichobezoars large enough to require surgical excision.5 Other psychiatric disorders — anorexia nervosa, obsessive compulsive disorder, pica, and depression — are also associated with Rapunzel syndrome. Nonpsychiatric causes include previous gastric surgery, prolonged gastric emptying, gastroparesis, reduction of gastric acid secretion, and diabetes mellitus.6
Most cases of Rapunzel syndrome are diagnosed late, owing to nonspecific symptoms in the early stages and low index of suspicion by the physician. Patients with trichobezoar usually present with abdominal pain, nausea, vomiting, gastric ulcers, hematemesis, perforation, and intestinal obstruction.3 Decomposition and fermentation of food residue results in severe halitosis. Patients may also present with a palpable abdominal mass. Physical examination may reveal patchy alopecia; 62% of patients present with anemia. Complications vary and can include episodes of incomplete pyloric stenosis, complete bowel obstruction, peritonitis, and death.7 Gastrointestinal perforation and peritonitis are the cause of mortality in 30% of cases. Other complications include acute pancreatitis, hypoalbuminemia, iron deficiency / megaloblastic anemia, and protein-losing enteropathies.
Different imaging modalities can aid diagnosis of Rapunzel syndrome. Ultrasonography reveals a hypoechoic, intraluminal mass with an arc-like surface and dense acoustic shadowing. Abdominal CT shows a well-circumscribed lesion composed of concentric whorls of different densities with multiple pockets of air enmeshed within. Oral contrast fills the stomach lumen while the absence of contrast enhancement precludes a neoplastic lesion. CT is also performed to gauge the extent of the bezoar and possible complications. Abdominal magnetic resonance imaging can also show a large mass of hypointense signal in the stomach on all pulse sequences and shaped according to the gastric lumen with extension into the small intestine. Gastro-duodenal endoscopy remains the gold standard for diagnosing Rapunzel syndrome. On endoscopy, a trichobezoar appears as a black or dark brown to greenish intragastric mass with a slimy sticky surface and a putrid odor owing to decomposition of various organic residues interspersed with hair.8
Treatment includes surgical removal of large trichobezoars through gastrostomy or upper-abdominal laparotomy. Endoscopic/laparoscopic removal is often possible for small trichobezoars. Noninvasive methods, such as enzymatic dissolution by pancreatic lipase or cellulose, and medical treatment with metoclopramide or acetyl cysteine have low success rates.9 Recurrence after surgical removal has been reported in the literature; prevention consists of managing underlying psychiatric illness and long-term follow-up.
CONCLUSION
Rapunzel syndrome, a large gastric trichobezoar causing transient intussusception, is a very rare phenomenon. The diagnosis should be considered in patients with history of trichophagia. The treatment of choice is surgical removal of the mass and psychiatric treatment accompanied by behavior therapy to prevent recurrence.
References
- Vaughn ED Jr., Sawyers JL, Scott HW Jr. The Rapunzel syndrome-an unusual complication of intestinal bezoar. Surgery. 1968; 63:339-343.
- Grimm Brothers: Rapunzel. Translated by Godwin-Jones R., Richmond, Virginia Common Wealth University Department of Foreign language; 1994-1999.
- Naik S, Gupta V, S Naik, Rangole A, Chaudhary AK, P Jain, et al. Rapunzel syndrome reviewed and redefined. Dig Sur. 2007; 24:157-161.
- Shorter E. A historical dictionary of psychiatry. New York: Oxford University Press; 2005.
- Irving PM, Kadirkamanathan SS, Priston AV, Blanshard C. Education and imaging. Gastrointestinal: Rapunzel syndrome. J Gastroenterol Hepatol. 2007; 22:2361.
- Chojnacki KA. Foreign bodies and bezoars of the stomach and small intestine. In: Yeo CJ, Dempsey DT, Peters JH, editors. Shackelford’s Surgery of the Alimentary Tract. 6th ed. Philadelphia: Saunders Elsevier; 2007; 940–46.
- Mohite PN, Gohil AB, Wala HB, Vaza MA. Rapunzel syndrome complicated with gastric perforation diagnosed on operation table. J Gastrointest Surg. 2008;12 (12):2240-2242.
- Sharma UK, Sharma Y, Chhetri RK, Makaju RK, Chapagain S, Shrestha R. Epigastric mass in a young girl: Trichobezoar: Imaging Diagnosis. Nepal Med Coll J. 2006; 8:211-212
- Coulter R, Antony MT, Bhuta P, Memon MA. Large gastric trichobezoar in a normal healthy woman: case report and review of pertinent literature. South Med J. 2005; 98(10):1042-1044.
Affiliations: Dr. Ziauddin University Hospital, Karachi, Pakistan. The author declares no conflicts of interest.
