Amyand Hernia Complicated by Acute Appendicitis
Images


Case Summary
An elderly patient presented to the emergency department with acute right testicular pain and vomiting following a recent diagnosis of right inguinal hernia. In addition to the hernia, the physical exam was notable for tenderness in the right groin and scrotum.
Imaging Findings
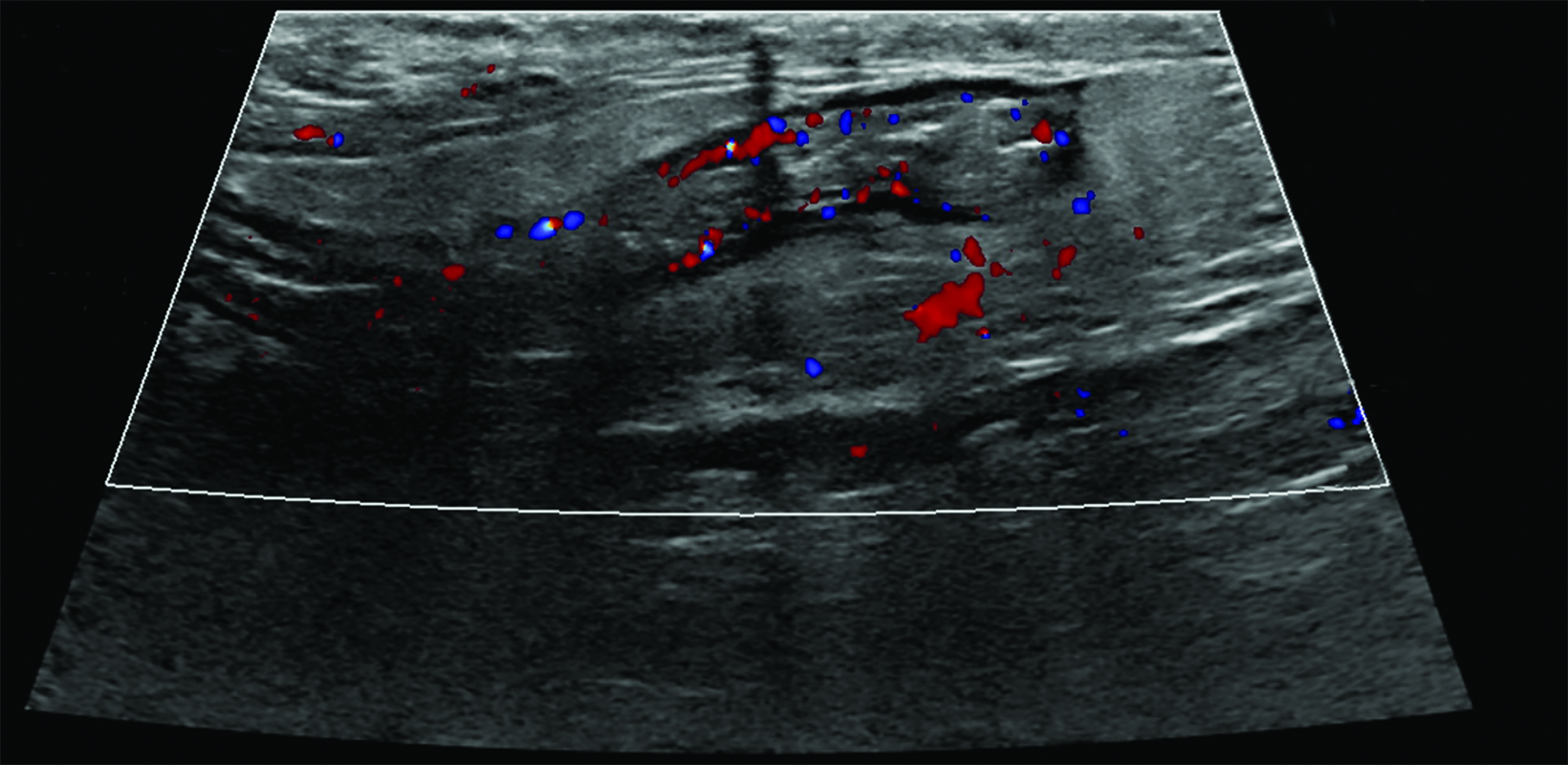
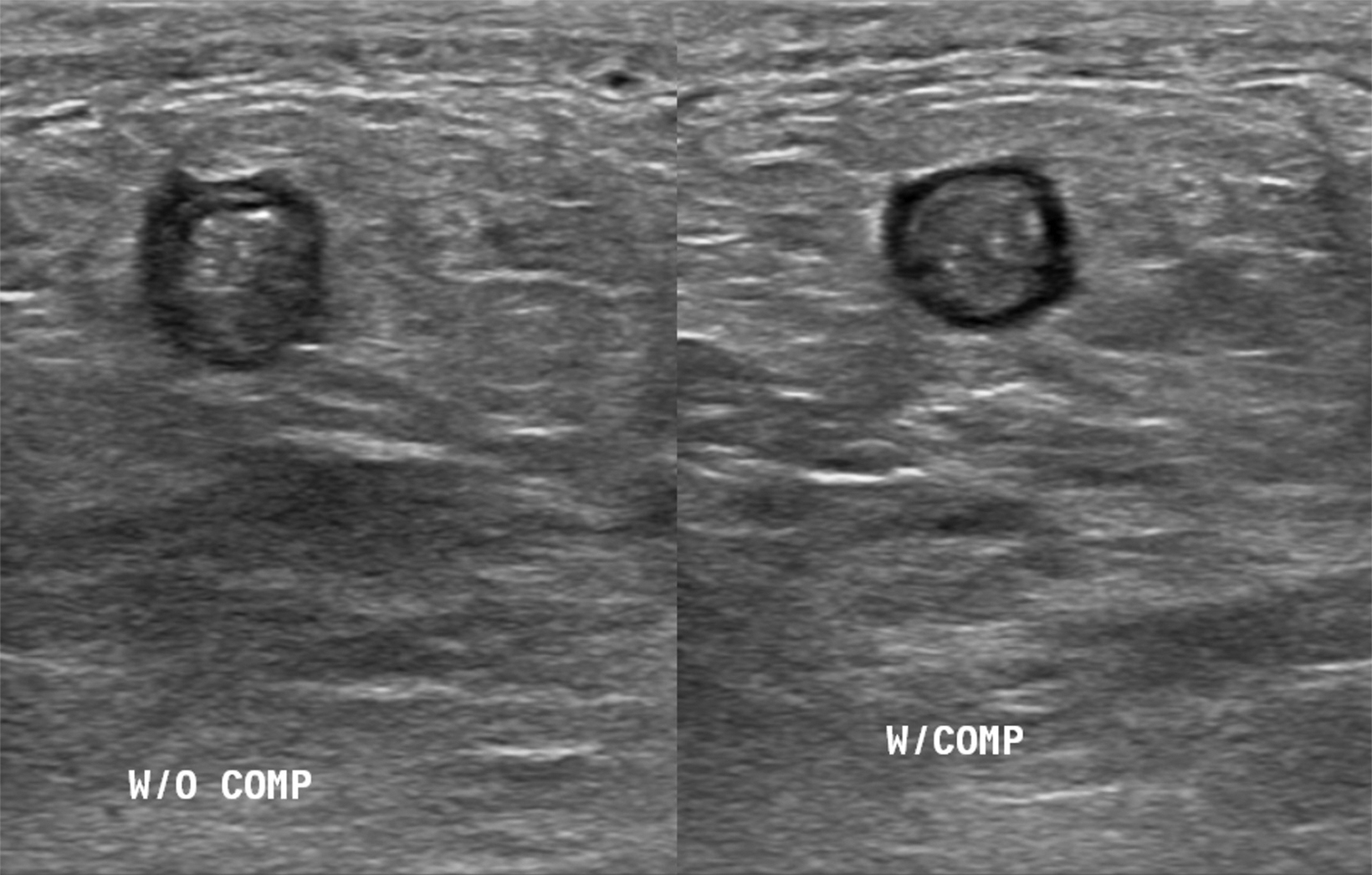
Scrotal ultrasound (Figures 1, 2) demonstrated a blind-ending, noncompressible tubular structure in the right inguinal canal, measuring up to 9 mm in diameter, with moderate peripheral color flow.
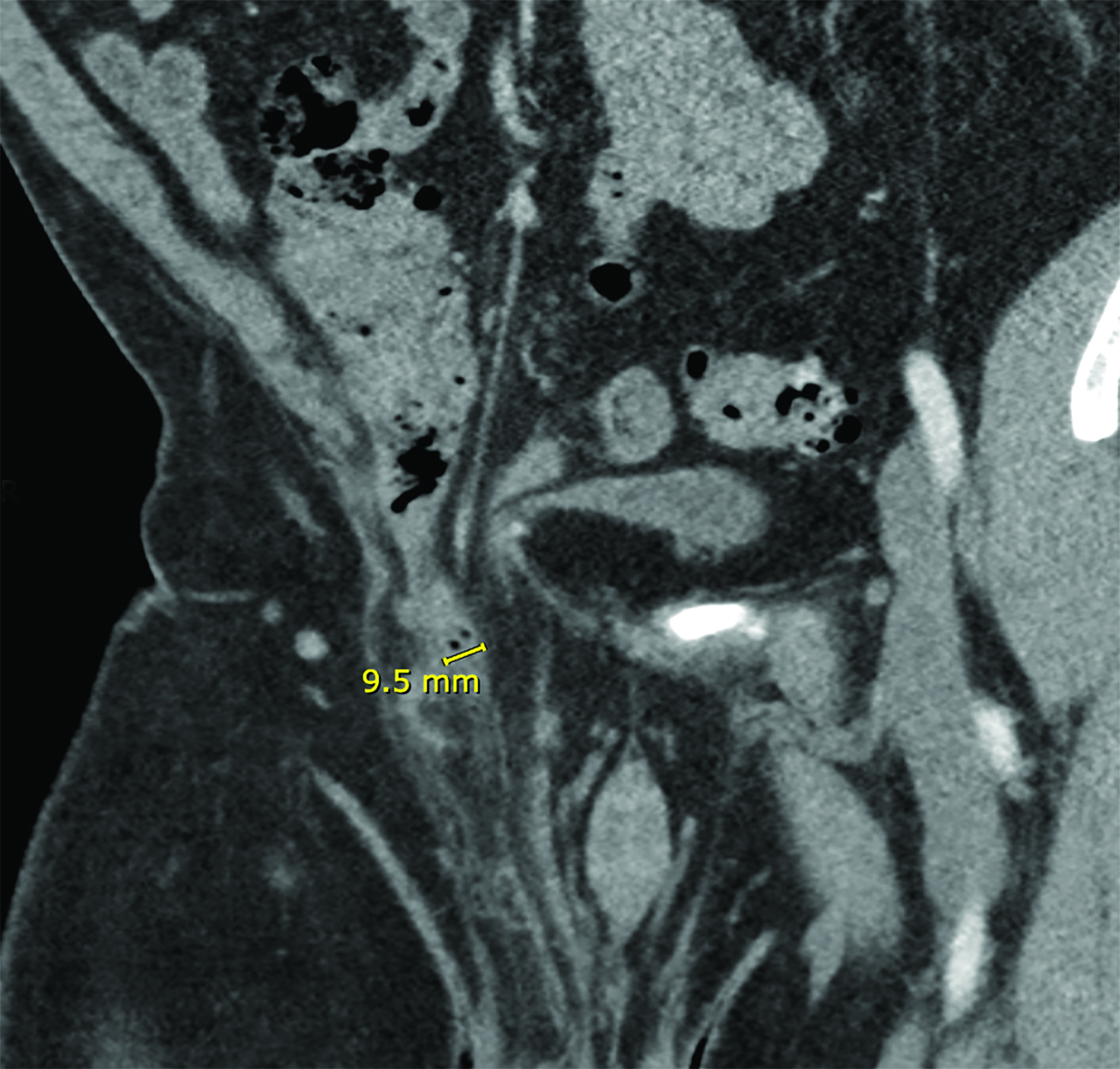
While scanning the spermatic cord, the sonographer noticed a tubular structure within the inguinal canal and proceeded to perform the scan with compression. The reading radiologist recommended abdominopelvic CT (Figure 3), which confirmed the presence of a noncompressible, inflamed appendix within the hernia. The appendix measured up to 10 mm and the proximal portion was found to be mildly thickened with mild surrounding inflammatory fat stranding.
Diagnosis
Amyand hernia with acute appendicitis.
The main differential diagnosis is a strangulated inguinal hernia, which can have a similar presentation.
Discussion
Amyand hernia is named for Claudius Amyand, the French surgeon who discovered an inflamed appendix within a right inguinal hernia sac while performing the first recorded successful appendectomy on an adolescent in 1735.1,2
Amyand hernia is rare, making up 0.19% to 1.7% of inguinal hernias; a 2003 study of 1,341 inguinal hernias found only 0.6% of cases contained the appendix.2-4 Amyand hernia can occur at any age but is up to 3 times more common in children than adults.5 Incidence of concurrent appendicitis is even more uncommon, occurring in an estimated 0.07-0.13% of inguinal hernias.4
Most cases are diagnosed at surgery, as imaging is not routinely performed prior to inguinal hernia repair. Incarceration of the appendix, however, is thought to be a predisposing risk factor for acute inflammatory changes that can prompt imaging.2
The pathophysiology of acute appendicitis in Amyand hernia is not clear. It is thought that extraluminal compression of the appendix inside the hernia, rather than intraluminal obstruction as seen in most cases of appendicitis, leads to ischemia, bacterial overgrowth, and inflammation within the appendix.6
Surgery is the mainstay of treatment. In most cases, the hernia is repaired concurrently with the appendectomy; however, this is at the surgeon’s discretion.2, 4 If the hernia is to be repaired with a mesh, the surgeon may choose to wait until the inflammation/ infection has resolved to repair the hernia.
Our patient underwent laparoscopic appendectomy and returned two months later for hernia repair with mesh placement.
Conclusion
Because Amyand hernia itself is rare, and imaging is not necessary prior to most inguinal hernia surgeries, preoperative diagnosis of the condition is exceedingly rare. On ultrasound, a blind-ending structure within the hernia sac should raise suspicion for Amyand hernia. To assess for acute appendicitis, compression and color flow ultrasound images should be obtained; CT may be performed to confirm the findings in equivocal cases. Treatment consists of surgery.
References
Citation
NA J, MJ P. Amyand Hernia Complicated by Acute Appendicitis. Appl Radiol. 2024;(3):36-38.
May 7, 2024