Advice from SPR about pediatric incidental pulmonary nodules
With the technological capabilities of CT scanners that can display lung nodules as small as 1-2 mm on scans of children that cover all or part of the chest, the frequency of identifying incidental pulmonary nodules that in previous years would never have been visible on diagnostic images increasing. How should radiologists react? What guidelines should they follow?
They shouldn’t follow the Fleischner guidelines for adults or automatically order a follow-up CT, according to the members of the Thoracic Imaging Committee of the Society for Pediatric Radiology (SPR). The committee published detailed recommendations in Pediatric Radiology as a precursor to the development of pediatric-specific guidelines.
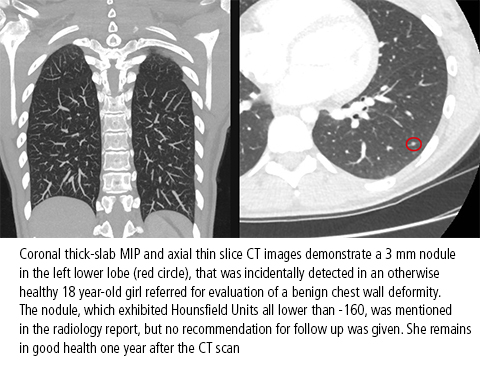 Small pulmonary opacities can be characterized as linear or as ground-glass or solid nodules. Linear opacities and ground glass nodules are extremely unlikely to represent an early primary or metastatic malignancy in a healthy child, lead author Sjirk J. Westra, M.D., a pediatric radiologist at Massachusetts General Hospital in Boston and committee co-authors advised. They do not recommend ordering a routine follow-up CT scan, noting that the radiation exposure may cause more harm than benefit.
Small pulmonary opacities can be characterized as linear or as ground-glass or solid nodules. Linear opacities and ground glass nodules are extremely unlikely to represent an early primary or metastatic malignancy in a healthy child, lead author Sjirk J. Westra, M.D., a pediatric radiologist at Massachusetts General Hospital in Boston and committee co-authors advised. They do not recommend ordering a routine follow-up CT scan, noting that the radiation exposure may cause more harm than benefit.
The authors provide detailed descriptions of nodule characteristics associated with diagnosis of pediatric lung cancer and other types of thoracic malignancies. Based on detailed research and review of existing literature, they comment that:
- Linear opacities should not be considered solid nodules, as they are more likely related to prior infection, inflammation, or atelectasis.
- Ground-glass opacities are very unlikely to represent a malignancy in an asymptomatic child without a history of malignancy. They tend to be caused by infection or inflammation. Additionally, the presence of the halo sign of ground-glass opacity surrounding a solid pulmonary nodule is often indicative of an aggressive lesion with hemorrhage or infiltration in the adjacent lung parenchyma. It is very unlikely to be encountered in lung nodules detected incidentally. Additionally, malignant lung nodules in children are more likely to be caused by metastatic disease than by a primary lung tumor.
- When a nodule is identified in the scans of children with a history of congenital pulmonary airway malformation, immune deficiency, or malignancy, it should not be considered incidental and should be further investigated.
The article also includes pragmatic advice on how and what to say to a patient’s family. They point out that fewer incidental pulmonary nodules would be discovered if more clinicians were more rigorous in deciding whether to order a CT exam for a pediatric patient. And, if one is ordered, they recommend that a strategy to follow is to purposefully avoid scanning parts of the lung when adjacent regions are scanned. “This strategy requires us to have a more active role in the protocol of studies and the real-time review of preliminary findings when our patients are on the scanner, to decide whether the clinical question has been adequately addressed, or whether there is an indication to extend the scan coverage over adjacent regions such as the chest,” the authors note.
REFERENCES
- Wekstra SJ, Brody AS, Mahani MG, et al. The incidental pulmonary nodule in a child. Part 1: Recommendations from the SPR Thoracic Imaging Committee regarding characterization, significance and follow up. Pediatr Radiol. 2015;45(5):628-633.
- Wekstra SJ, Brody AS, Mahani MG, et al. The incidental pulmonary nodule in a child. Part 1: Commentary and suggestions for clinical management, risk communication and prevention. Pediatr Radiol. 2015;45(5):634-639.