Acute Adrenal Hemorrhage
Case Summary
An elderly patient with a history of atherosclerosis, atrial fibrillation, hyperlipidemia, and pacemaker placement presented to the emergency department with right-sided pain below the breast. This pain began 1 hour earlier while the patient was operating construction equipment. The patient also complained of chest pain, nausea, and vomiting. The patient’s blood pressure was 67/52 and heart rate was 67 bpm, with otherwise normal vital signs. Physical examination was significant for a diaphoretic patient with severe right upper quadrant tenderness. CT abdomen and pelvis with intravenous contrast was performed, followed by abdominal aortography.
Imaging Findings
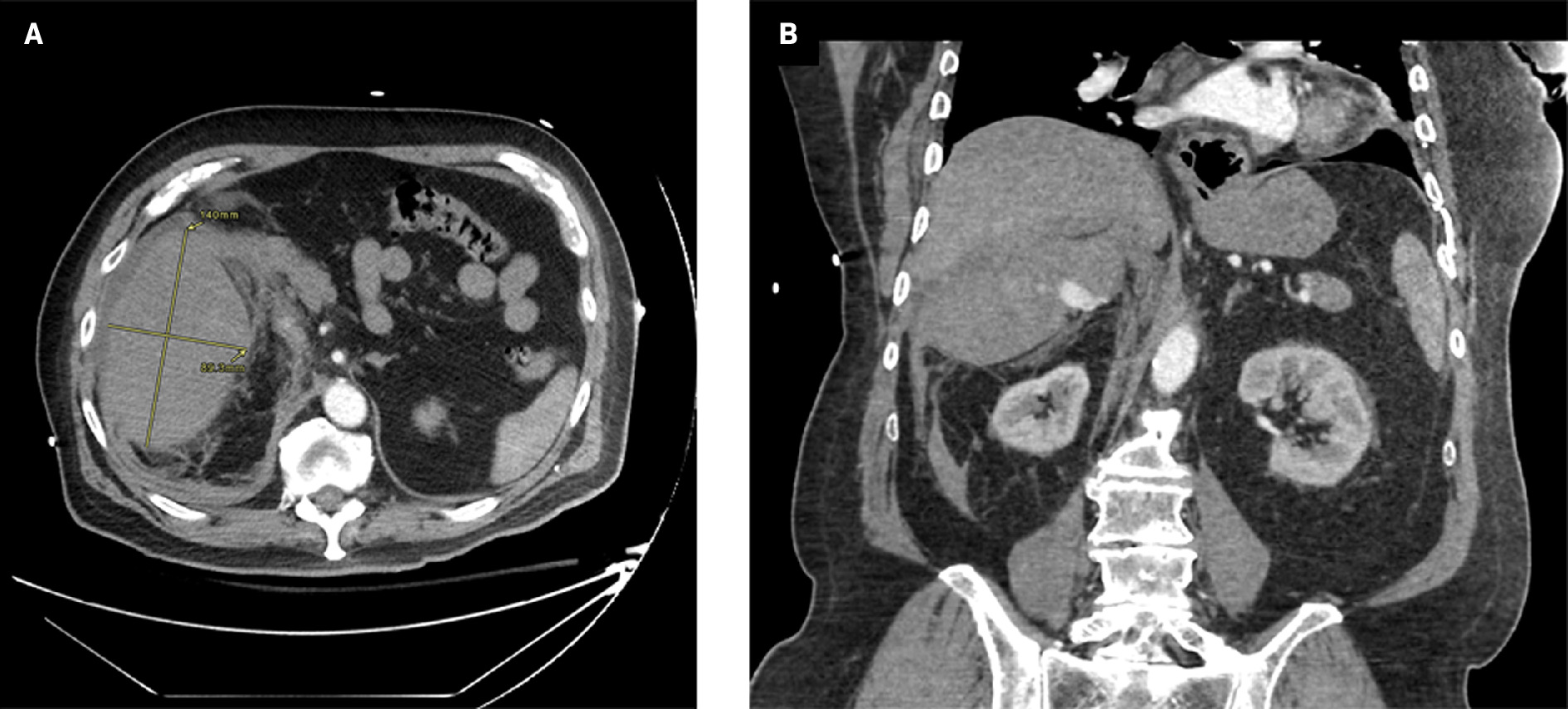
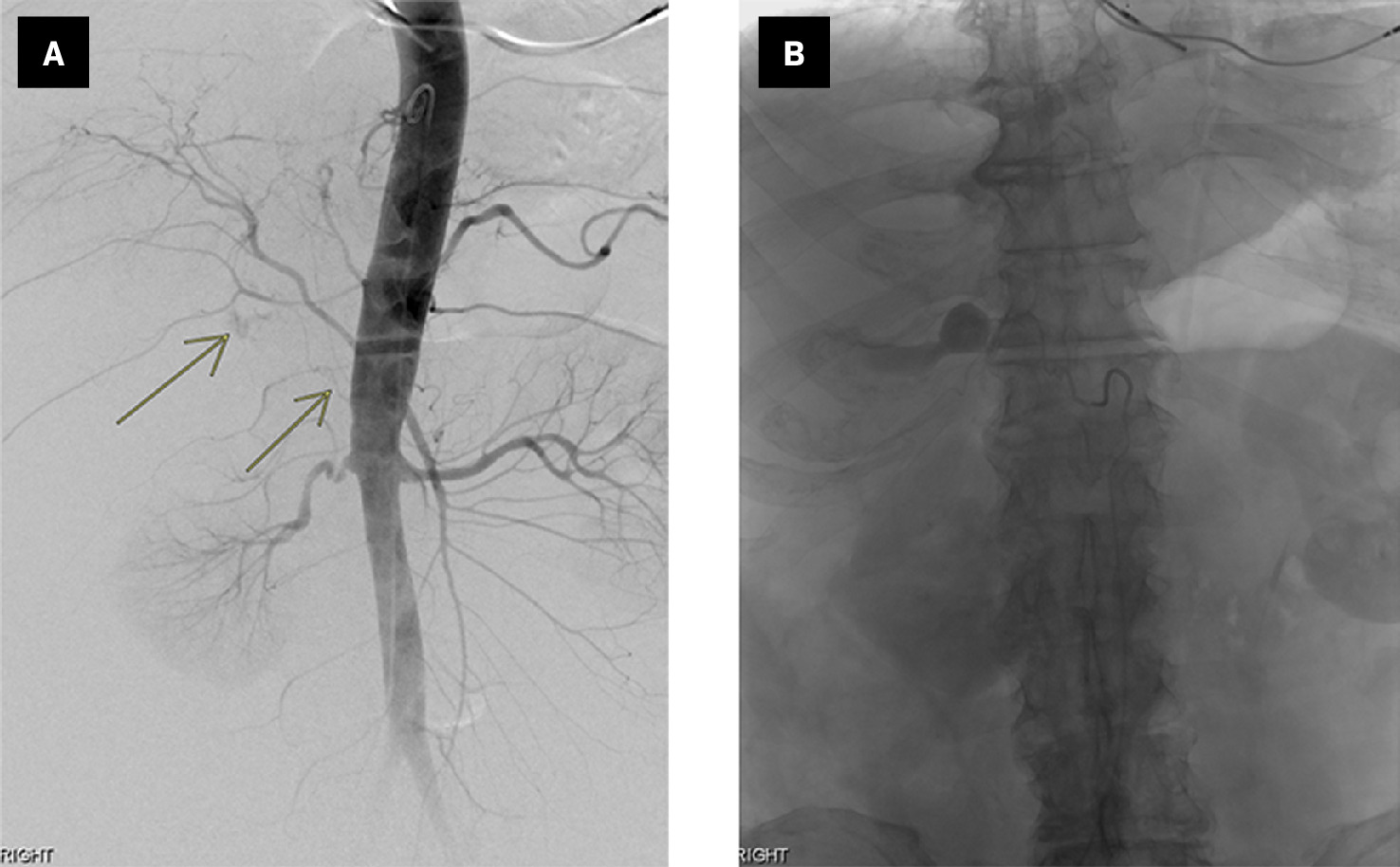
Abdominal and pelvis CT ( Figure 1 ) demonstrated a hemorrhagic soft-tissue mass in the right upper quadrant of the abdomen arising from the adrenal gland. A rapidly perfused pseudoaneurysm within the mass was also evident. A subsequent abdominal aortogram ( Figure 2 ) revealed contrast extravasation from the middle adrenal artery correlating to the area on the CT. Subsequent coil embolization of the right middle adrenal artery proximal to the pseudoaneurysm was performed.
Axial CT ( A ) through the upper abdomen shows a 14 × 9-cm hemorrhagic soft-tissue mass in the right upper quadrant of the abdomen. Coronal view ( B ) shows avid contrast in the pseudoaneurysm within the hemorrhage.
Anteroposterior view ( A ) from an abdominal aortogram depicts the middle adrenal artery originating from the aorta with active extravasation (arrows), correlating to the area of pseudoaneurysm on CT. Selective right middle adrenal arteriography ( B ) of the pseudoaneurysm shows the middle adrenal artery with contrast extravasation from the pseudoaneurysm.
Diagnosis
Acute adrenal hemorrhage with pseudoaneurysm
Discussion
Adrenal hemorrhage is an uncommon condition characterized by bleeding into the suprarenal glands. It is estimated to be present in approximately 0.14% to 1.8% of postmortem examinations.1 The actual incidence may be higher as the condition’s vague symptoms, comorbid conditions, and variable laboratory findings can make diagnosis challenging. Adrenal hemorrhage is more common in men, likely owing to increased frequency of underlying causes. It can affect neonates and middle-aged individuals.2 While hemorrhage severity depends on the etiology, the condition overall carries an approximate 15% mortality rate. In patients with Waterhouse-Friderichsen syndrome (often caused by meningococcal sepsis), the mortality rate is 55% to 60%.3
The etiology of adrenal hemorrhage is diverse and can be classified as primary (idiopathic) or secondary to abdominal trauma, infection, septicemia, anticoagulant use, pregnancy, acute stress, neonatal stress, surgery, neoplasm, or autoimmune disease.
Imaging remains the most important diagnostic tool; CT is the modality of choice. Acute hemorrhage typically appears as a nonenhancing mass with low or mixed attenuation observed in one or both adrenal glands. Normal adrenal contrast enhancement may still be present, especially in a peripheral distribution. Sometimes, a train-track appearance is noted, where peripheral enhancement is preserved with central low attenuation.4 Other features that may be seen include periadrenal fat stranding and active extravasation with bleeding into the retroperitoneal area.
MRI can display high T1 signal intensity or rapidly changing signal and is the most accurate modality for differentiating acute from chronic hematomas, as well as demonstrating the presence of an underlying tumor. Bleeding may continue until the adrenal gland expands beyond its original shape, forming a round or oval hematoma from a few centimeters to more than 10 cm.4, 5 In infants, ultrasound is the modality of choice due to their small body size and relatively large adrenal size.2 Blood loss may be associated with abnormal lab parameters such as leukocytosis and anemia. Hyponatremia, hyperkalemia, and hypoglycemia may also be detected if there is adrenal insufficiency.5
Treatment depends on the extent of the hemorrhage and the degree of hormonal insufficiency. Patients with hemodynamic instability refractory to transfusion or rapidly expanding hemorrhagic masses are candidates for intervention.6 Angiography and embolization of the bleeding lesion, as in this case. In the acute setting, excluding an adrenal tumor can be challenging and delayed imaging is usually required.7
Conclusion
Adrenal hemorrhage is a rare condition that can lead to acute adrenal insufficiency and may be fatal. The condition can present in a myriad of clinical contexts and with vague clinical features. Therefore, a high index of clinical suspicion and early diagnostic workup are required for prompt management and improved prognosis.
References
Citation
Lim J, Lee S, Mansilla A.Acute Adrenal Hemorrhage. Appl Radiol. 2024; (6):44 - 46.
doi:10.37549/AR-D-24-0046
December 1, 2024