Intraluminal esophageal diverticulum
By Mohammed AA, Diegnan B, Kanzaria P


CASE SUMMARY
A 74-year-old female presented to the hospital with nausea and vomiting. Three days ago, the patient felt food sticking in her throat after she ate apple pie, following which she started having nausea and vomiting. She was not able to eat or drink much after that episode but she continued to have episodes of nausea. The patient had similar symptoms when she was diagnosed with esophageal stricture several years ago. The esophageal stricture was thought to be secondary to severe GERD. She had past endoscopic dilatation twice, following which her symptoms improved, but she has not had recent esophageal dilatation.
Physical examination was unremarkable. Laboratory test results were normal. Single contrast barium swallow was performed.
IMAGING FINDINGS
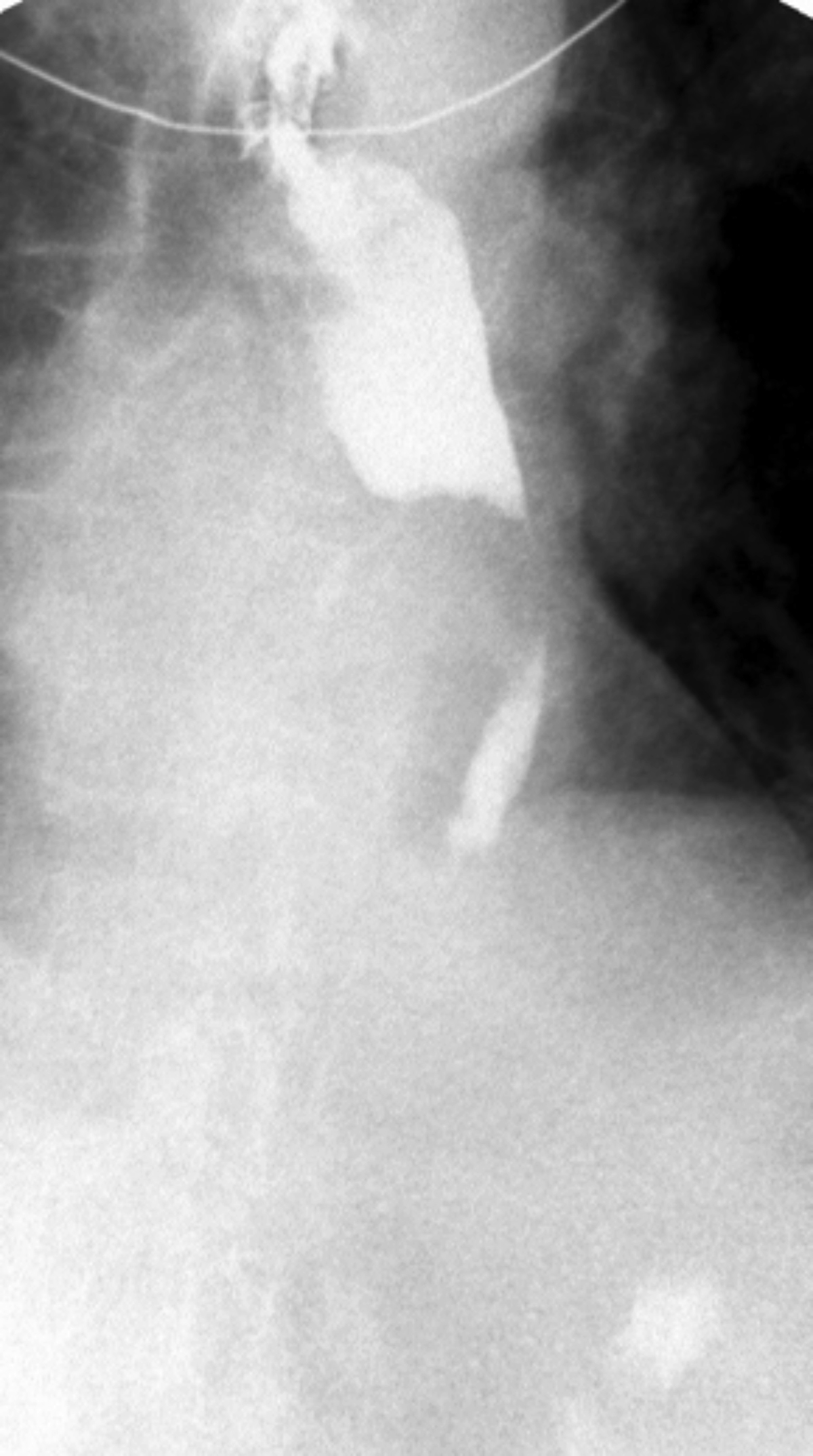
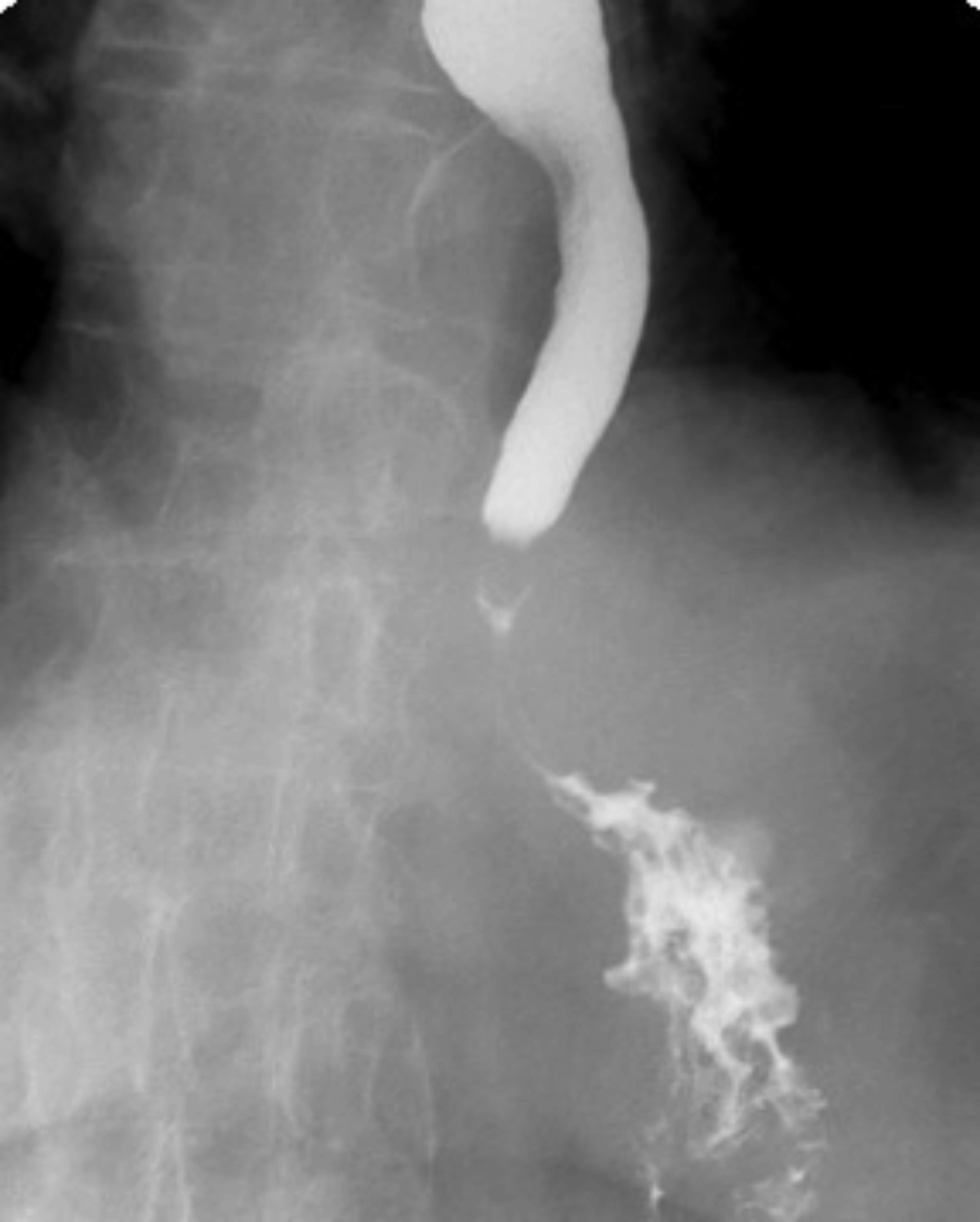
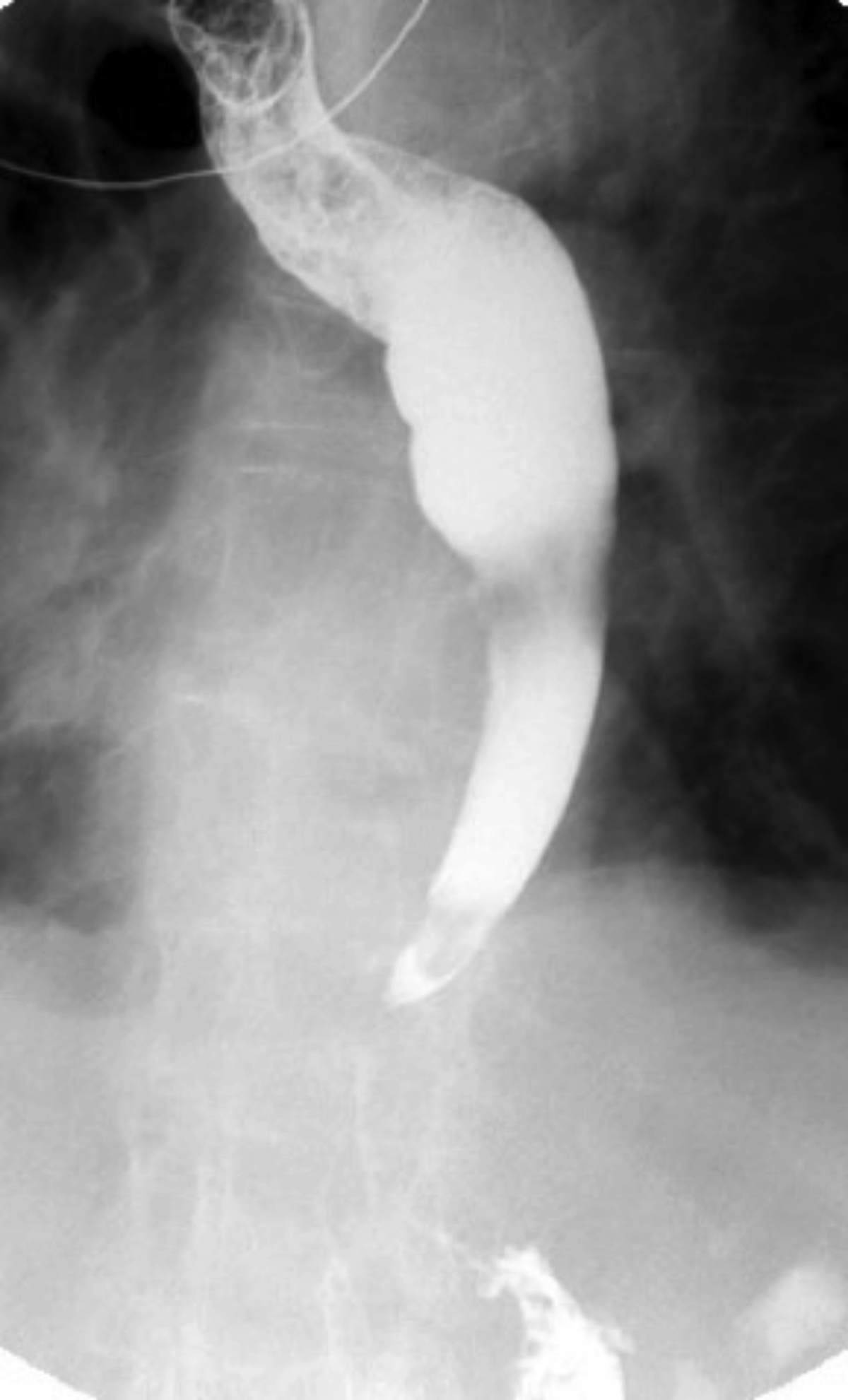
Single contrast barium swallow revealed a tortuous esophagus (Figure 1) causing the contrast to flow slowly down the esophagus (Figure 2). In the mid esophagus, there is a large collection of intraluminal barium with surrounding radiolucent halo (Figure 3). Distal to this collection, the esophagus is narrowed (Figure 4). There is likely narrowing of the gastroesophageal junction. There was passage of a small amount of contrast into the stomach. The majority of the barium remained in the esophagus after 10 minutes of examination (Figure 5).
DIAGNOSIS
Intraluminal esophageal diverticulum
DISCUSSION
Intraluminal esophageal diverticulum is a rare entity that was first described radiologically by Nelson in 1947.1 Intraluminal esophageal diverticulae are usually related to mucosal damage secondary to increased intraluminal pressure.2 There is a pouch of mucosal membrane that is open proximally and closed distally.3 Although they may be congenital, intraluminal esophageal diverticulae tend to be acquired lesions related to mucosal damage secondary to increased intraluminal pressure in the esophagus that has been narrowed by an inflammatory process.4
In our case, a large collection of intraluminal barium with surrounding radiolucent halo (Figure 3) and distal esophageal narrowing (Figure 4) was demonstrated on barium swallow, indicating the existence of the diverticular structure which communicated with the esophageal lumen.
The concept of intraluminal esophageal diverticulum (IED) was presented by Schreiber and Davis in 1977.3 They reported the first two cases of IED. Grand and L’Hermin reported another case of IED.5 In these cases, radiological findings were not reproducible on repeat barium meals and no diverticula were found by esophagoscopy.6
Cho et al7 reported three additional cases and considered this finding as a transient artifactual phenomenon created by the interface of the barium bolus with the viscous secretion or air.6 The same radiological artifactual phenomena were observed in the stomach.10-13
It has been suggested that IED is caused by a partial esophageal web, which elongates distally with propulsive peristaltic pressure and forms a pocket-like structure within the esophageal lumen. The congenital or acquired mucosal weakness of the esophageal wall may be another contributing factor as mentioned.3,5 6,8
The radiological findings of IED are identical to those of intraluminal diverticula of other parts of the alimentary tract.9 An intraluminal barium collection surrounded by a radiolucent halo is a characteristic finding. A transient radiological artifact closely resembling IED is the important differential diagnosis with a true lesion. True IED is reproducible on repeat barium study and is recognized at endoscopic examination.6
CONCLUSION
Intraluminal esophageal diverticulum is a rare entity that was first described radiologically by Nelson in 1947. Intraluminal esophageal diverticulae are usually related to mucosal damage secondary to increased intraluminal pressure. There is a pouch of mucosal membrane that is open proximally and closed distally. Although they may be congenital, intraluminal esophageal diverticulae tend to be acquired lesions related to mucosal damage secondary to increased intraluminal pressure in the esophagus that has been narrowed by an inflammatory process.
REFERENCES
- Nelson, W. I. Congenital diaphragm of the duodenum; case report with preoperative x-ray studies. Minnesota Medicine. 1947(30.7):745-752.
- Eisenberg, Ronald L. Clinical imaging: an atlas of differential diagnosis. Lippincott Williams & Wilkins, 2010. 5th ed.
- Schreiber, M. H., and M. Davis. Intraluminal diverticulum of the esophagus. American Journal of Roentgenology. 1977;129.4:595-597.
- Eisenberg, Ronald L. Gastrointestinal radiology: a pattern approach. Lippincott Williams & Wilkins, 2003
- Grand, M., and C. L’Herminé. Diverticule intraluminal de l’cesophage. A propos d’un cas. J Radiol. 1980;61:131-133.
- Funakoshi, Osamu, et al. Intraluminal esophageal diverticulum. Gastroenterologia Japonica. 1990;25.1:117-121.
- Cho, Shao-Ru, et al. Vanishing intraluminal diverticulum of the esophagus. Gastrointestinal Radiology. 1982;7.1:315-317.
- Waldmann, H. K., and A. Turnbull. Esophageal webs. The American Journal of Roentgenology, Radium Therapy, and Nuclear Medicine. 1957;78.4:567-573.
- Mosimann, François, and Michel Bugnion. Intraluminal jejunal diverticulum. Gastrointestinal Radiology. 1981;6.1:309-311.
- Shackelford, Gary D. Barium collections in the stomach mimicking intraluminal diverticula. American Journal of Roentgenology. 19082;139.4:805-806.
- Tan, K. M. Intraluminal diverticula of the stomach. American Journal of Roentgenology. 1979;132.3:461-462.
- Beeckman, P. Vanishing diverticula of the stomach. AJR, American Journal of Roentgenology. 1979;133.5:996.
- Borgstrom, K. E. Ein Bariumkontrastph~ nomen bei der R6ntgenuntersuchung des Magens. Radiologe 3. 1963:384-385.
Prepared by Dr. Mohammed while a Diagnostic Radiology Resident; Dr. Diegnan while a Diagnostic Radiology Resident; and Dr. Kanzaria while a Radiologist at St. Vincent Hospital, Worcester, MA.
