Iatrogenic Neonatal Calcinosis Cutis
Images



Case Summary
A premature neonate presented to the emergency department at several weeks of age, for evaluation of a right arm mass, which was present for several days (Figure 1). The infant was afebrile and alert. The mass was located at the right antecubital fossa and was erythematous, nodular, and firm. Laboratory results on arrival revealed no leukocytosis or neutrophilia. The neonate had been discharged from the neonatal intensive care unit (NICU) several days before the appearance of the mass. In the NICU, the patient had been treated for hypocalcemia with calcium gluconate via peripheral IV placed in the right antecubital fossa.
Imaging Findings
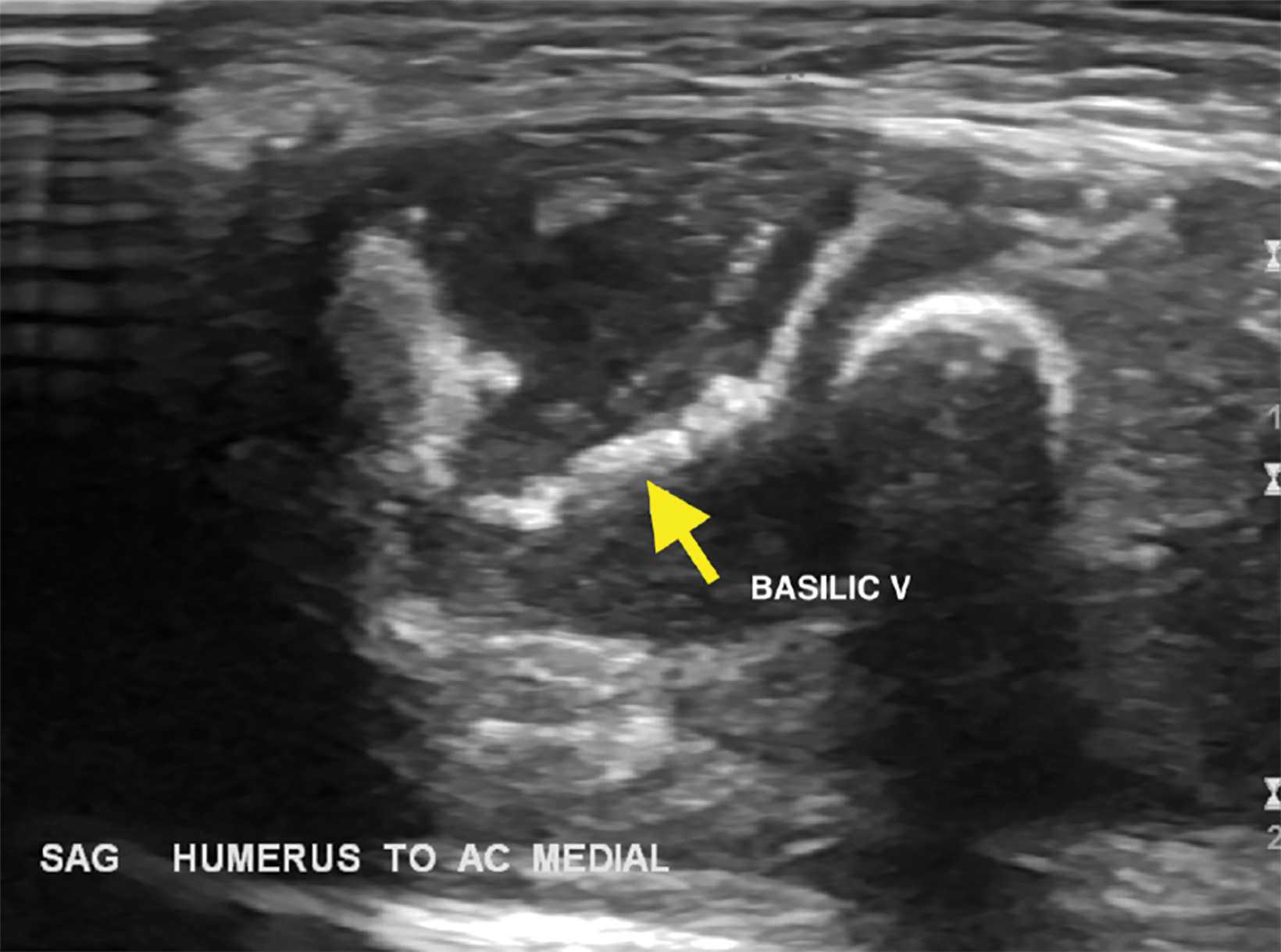
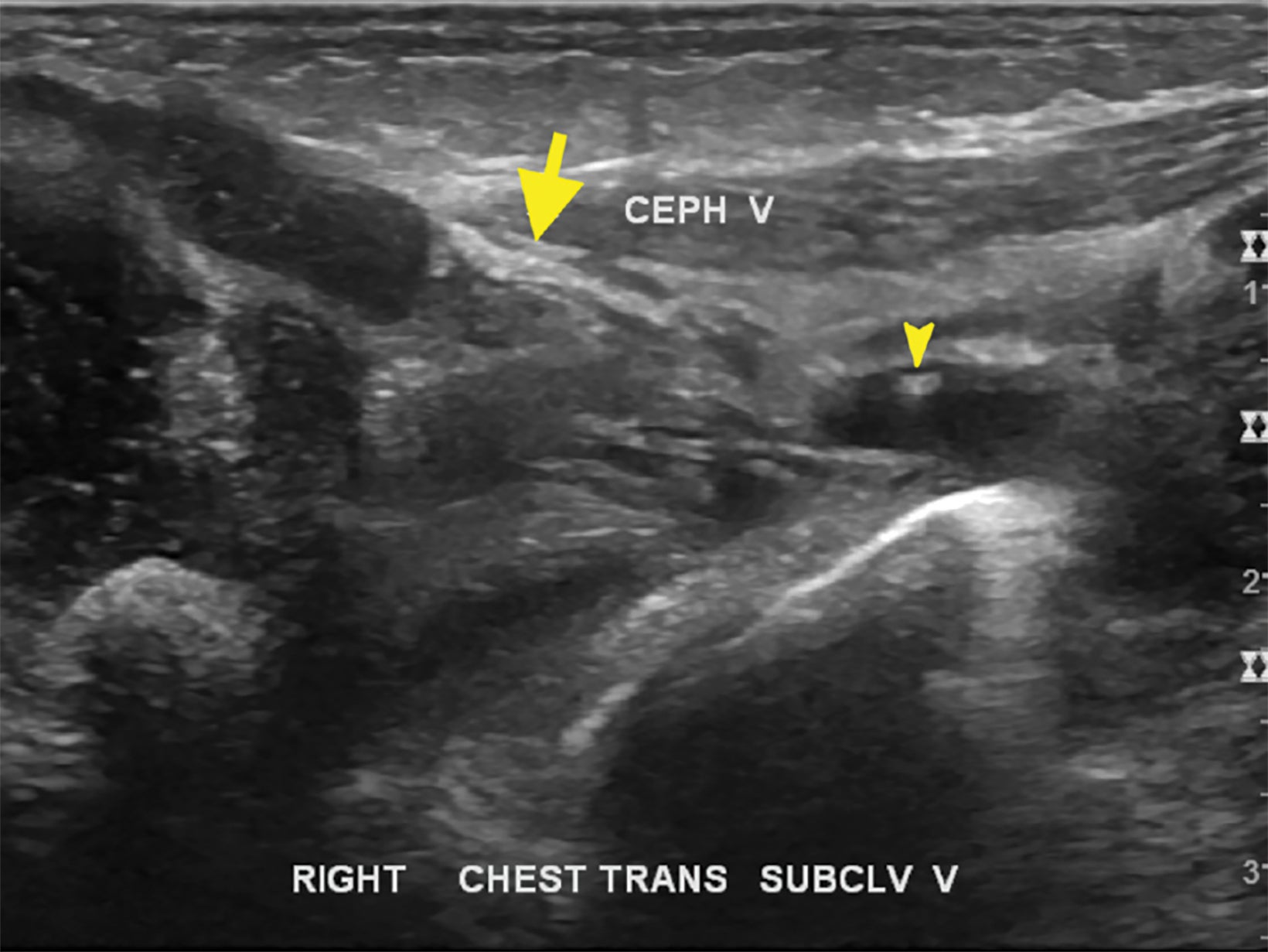
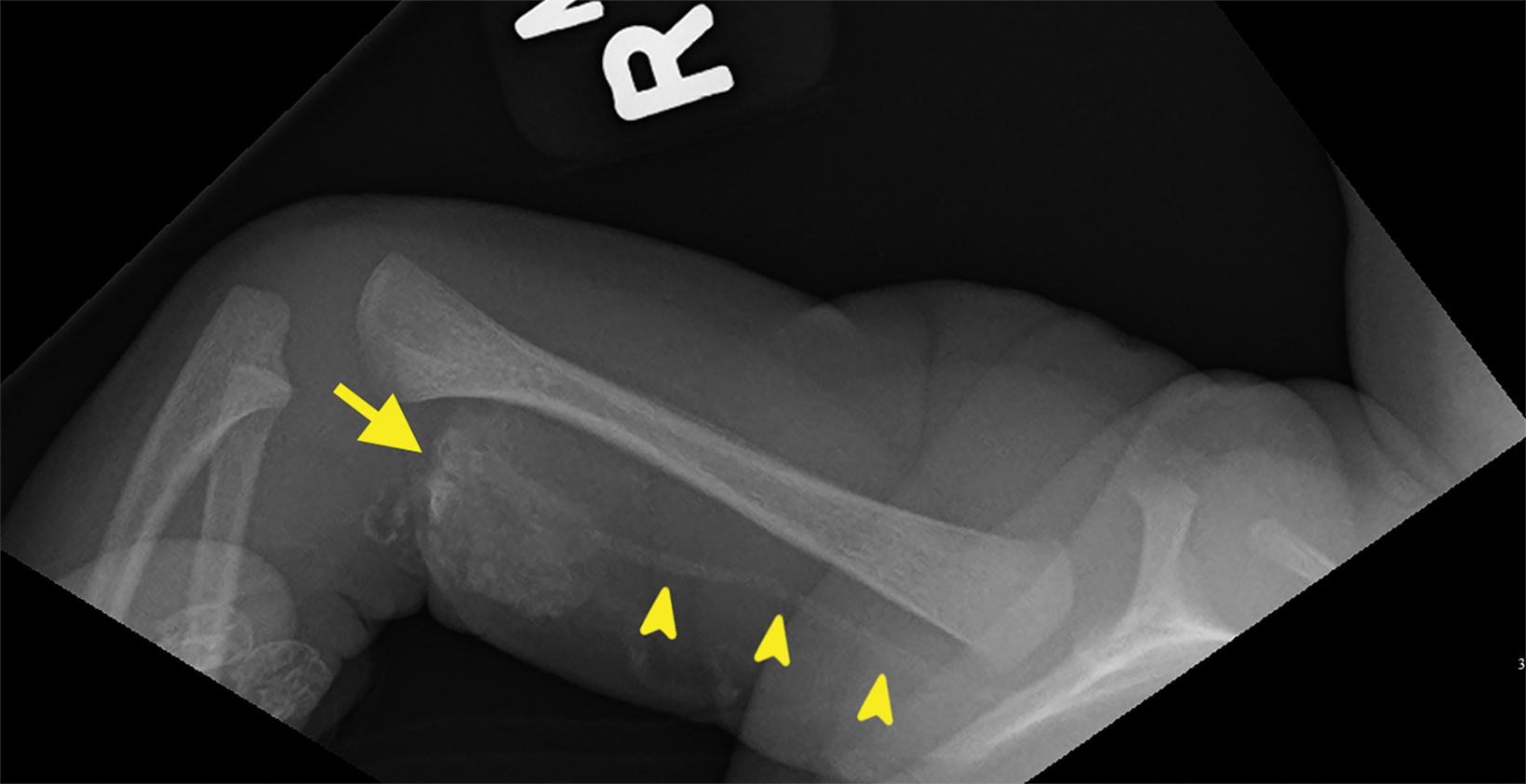
Sonographic images demonstrated a well-circumscribed, heterogeneous mass containing calcification with posterior shadowing and no abnormal internal vascularity (Figure 2). The cephalic and basilic veins were hyperechoic with posterior shadowing consistent with complete calcification, and a small, partially calcified, nonocclusive thrombus was seen in the right subclavian vein. Right humeral radiography demonstrated a calcific density in the antecubital region with high density material coursing along a path suggestive of venous structures, confirming the sonographic findings of the calcified cephalic and basilic veins (Figure 3).
Diagnosis
Iatrogenic neonatal calcinosis cutis. Differential diagnosis based on the imaging findings include subcutaneous fat necrosis of the newborn, subepidermal calcified nodule, osteoma cutis, pilomatricoma (calcifying epithelioma of Malherbe), and pseudoxanthoma elasticum.
Discussion
Calcinosis cutis results from the deposition of insoluble calcium salts into the skin and subcutaneous tissues. It can be separated into five subtypes: dystrophic calcification, metastatic calcification, calciphylaxis, idiopathic calcification, and iatrogenic calcification.1 Dystrophic calcification presents with cutaneous ectopic calcified masses composed of hydroxyapatite and calcium phosphate. Necrotic cells with denatured phosphate bound proteins become a nidus for calcification while altered collagen and elastin also facilitate calcification.2 High mitochondrial calcium and phosphate levels contribute to subsequent crystal deposition and necrosis, which results in a more acidic environment. Increased acidity subsequently interferes with calcification inhibitors.3
Dystrophic calcification is classically seen in connective tissue disorders; however, it can also manifest after local tissue injury or within tumors. Localized dystrophic calcification can be seen in scleroderma, while widespread calcification can be seen in juvenile dermatomyositis and is termed calcinosis universalis.3
Metastatic calcification results from abnormally elevated serum calcium or phosphate levels, which cause calcium salt precipitation in normal tissue. Milk alkali syndrome, excessive ingestion of calcium-containing foods or antacids, or hypervitaminosis D may result in metastatic calcification with cutaneous lesions regressing if serum calcium levels return to normal limits.4
Calciphylaxis is characterized by mural small-vessel calcification, predominantly within the subcutaneous fat or dermis, which leads to vasculopathy and eventually ischemia or infarction of the supplied tissue. Extravascular calcium deposits may also occur.5 Calciphylaxis most often presents in patients with end-stage renal disease; however, it has also been described in patients with normal renal function with primary hyperparathyroidism.6
The absence of an identifiable metabolic disorder, tissue damage, or therapy characterizes the idiopathic subtype. An example of idiopathic calcinosis cutis is tumoral calcinosis, a condition typified by the deposition of calcium around major joints in adolescents without underlying conditions or altered calcium metabolism.1
The iatrogenic subtype is usually seen as a side effect of therapy and has been reported to occur following the administration of intravenous calcium gluconate for hypocalcemia.7-13 In our patient, further testing revealed the mother to be vitamin D deficient, a risk factor predisposing newborns to neonatal hypocalcemia.11
Iatrogenic calcinosis cutis can develop after extravasation of calcium at a venipuncture site.1 Damaged subcutaneous tissue and resulting cell necrosis at the site of the extravasation creates a more acidic environment that lacks calcification inhibitors, facilitating precipitation.4 Multiple white-yellow cutaneous papules or nodules with erythema or necrosis develop within 3 weeks of the initial soft tissue injury.12
Calcification may also occur along blood-vessel sheaths from the extravasated material. In our patient, thrombosis was attributed to venous stasis resulting from calcification. Intravenous therapeutic calcium solutions are not radiodense; thus, radiographs do not typically show subcutaneous calcification until approximately 2 weeks following extravasation. Treatment options have included elevation, cold compresses, local surgery, the topical glucocorticoid triamcinolone, and diltiazem, a calcium channel blocker. In most cases, the calcification begins to clear at 8 weeks, with resolution occurring by 6 months.7
Subcutaneous fat necrosis of the newborn (SCFN) is one of the entities in the differential diagnosis for a subcutaneous lesion in neonates. It is a transient disorder of the subcutaneous adipose tissues, most often occurring in infants with hypoxia or perinatal stress and is characterized by firm subcutaneous nodules.14 The mechanism of SCFN is currently unknown; however, SCFN is postulated to occur from a combination of local tissue hypoxia and mechanical stress and/or the enrichment of saturated fatty acids, which increases the tissue propensity for crystalization.15
Hypercalcemia can be seen in up to 25% of SCFN cases.16 While the proposed mechanisms of SCFN differ from iatrogenic calcinosis cutis, lesions may appear sonographically similar. Additionally, subepidermal calcified nodule is a differential consideration for a solitary nodule within this demographic. However, the former typically occurs in the head or neck and is classified as an idiopathic calcinosis cutis. Clinical history is essential in making the correct diagnosis in these cases.
Conclusion
Calcinosis cutis occurs when insoluble calcium salts are deposited in the skin and subcutaneous tissues. Neonatal iatrogenic calcinosis cutis is rare but can be seen in neonates in the setting of prior intravenous calcium gluconate administration and may be suspected with appropriate historical findings, such as a history of neonatal hypocalcemia.
References
- Reiter N, El-Shabrawi L, Leinweber B, Berghold A, Aberer E. Calcinosis cutis: part I. Diagnostic pathway. J Am Acad Dermatol. 2011;65(1):1-12; doi: 10.1016/j. jaad.2010.08.038
- Kim SY, Choi HY, Myung KB, Choi YW. The expression of molecular mediators in the idiopathic cutaneous calcification and ossification. J Cutan Pathol. 2008;35(9):826-31 doi: 10.1111/j.1600-0560.2007.00904.x
- Touart DM, Sau P. Cutaneous deposition diseases. Part II. J Am Acad Dermatol. 1998;39(4 Pt 1):527-44 doi: 10.1016/s0190-9622(98)70001-5
- Walsh JS, Fairley JA. Calcifying disorders of the skin. J Am Acad Dermatol. 1995;33(5 Pt 1):693-706; doi: 10.1016/0190-9622(95)91803-5
- Rivet J, Lebbé C, Urena P, et al. Cutaneous calcification in patients with end-stage renal disease: a regulated process associated with in situ osteopontin expression. Arch Dermatol. 2006;142(7):900-6 doi: 10.1001/archderm.142.7.900
- Pollock B, Cunliffe WJ, Merchant WJ. Calciphylaxis in the absence of renal failure. Clin Exp Dermatol. 2000;25(5):389-92 doi: 10.1046/j.1365-2230.2000.00671.x
- Arora A, Agarwal A, Kumar S, Gupta SK. Iatrogenic calcinosis cutis—a rare differential diagnosis of soft-tissue infection in a neonate: a case report. J Orthop Surg. (Hong Kong) 2005;13(2):195-8 doi: 10.1177/230949900501300218
- Berger PE, Heidelberger KP, Poznanski AK. Extravasation of calcium gluconate as a cause of soft tissue calcification in infancy. Am J Roentgenol Radium Ther Nucl Med. 1974;121(1):109-17 doi: 10.2214/ajr.121.1.109
- Chen TK, Yang CY, Chen SJ. Calcinosis cutis complicated by compartment syndrome following extravasation of calcium gluconate in a neonate: a case report. Pediatr Neonatol. 2010;51(4):238-41 doi: 10.1016/s1875-9572(10)60045-9
- Cherian EV, Shenoy KV, Daniel J. Iatrogenic calcinosis cutis in a neonate. BMJ Case Rep. 2013;2013 doi: 10.1136/bcr-2012-007793
- Moss J, Syrengelas A, Antaya R, Lazova R. Calcinosis cutis: a complication of intravenous administration of calcium glucanate. J Cutan Pathol. 2006;33 Suppl 2:60-2 doi: 10.1111/j.1600-0560.2006.00519.x
- Mu SC, Lin CH, Sung TC. Calcinosis cutis following extravasation of calcium gluconate in neonates. Acta Paediatr Taiwan. 1999;40(1):34-35.
- Sonohata M, Akiyama T, Fujita I, Asami A, Mawatari M, Hotokebuchi T. Neonate with calcinosis cutis following extravasation of calcium gluconate. J Orthop Sci. 2008;13(3):269-72 doi: 10.1007/s00776-007-1217-z.
- Stefanko NS, Drolet BA. Subcutaneous fat necrosis of the newborn and associated hypercalcemia: A systematic review of the literature. Pediatr Dermatol. 2019;36(1):24-30 doi: 10.1111/pde.13640
- Del Pozzo-Magaña BR, Ho N. Subcutaneous fat necrosis of the newborn: A 20-year retrospective study. Pediatr Dermatol. 2016;33(6):e353-e55 doi: 10.1111/pde.12973
- Muzy G, Mayor SAS, Lellis RF. Subcutaneous fat necrosis of the newborn: clinical and histopathological correlation. An Bras Dermatol. 2018;93(3):412-14 doi: 10.1590/abd1806-4841.20187508
Citation
C S, I A, AJ T, Towbin RB J K,. Iatrogenic Neonatal Calcinosis Cutis. Appl Radiol. 2023;(1):50-53.
February 1, 2023