Ultrasound of the acute scrotum
Images










Dr. Chen is an Associate Professor of Radiology and Dr. John is a Professor and the Chair of the Department of Diagnostic and Interventional Imaging, University of Texas Medical School at Houston, Houston, TX.
While acute scrotal pain is a common clinical problem in both children and adults, symptoms are often vague and clinical findings are nonspecific. Ultrasound (US) allows for expedient and accurate differentiation of many causes of scrotal pain, including prompt diagnosis of testicular torsion that helps maximize testicular viability. Advances in high-resolution gray-scale and color Doppler US have expanded the clinical applications of scrotal US and have made it the ideal imaging modality for evaluation of the acute scrotum in both children and adults.
Technique
Scrotal US is best performed with a linear 7.5- to 12-MHz transducer. A lower-frequency transducer may be helpful with marked scrotal swelling. Direct scanning with copious acoustic gel is performed most frequently, but a standoff pad may be useful for superficial abnormalities. A towel or the examiner's hand may be used to elevate and support the scrotal sac. In addition to imaging in the longitudinal and transverse planes, it is helpful to obtain simultaneous images of both testes for comparison. Color Doppler is used to evaluate for abnormalities of flow and to differentiate vascular from nonvascular lesions but may be hampered in the younger child by motion artifacts. Attention to appropriate color Doppler settings to optimize detection of slow flow is critical. Power Doppler is a useful adjunct to color Doppler in low-flow states, but it is more sensitive to motion artifacts. The Valsalva maneuver or scanning in the upright position should be performed when evaluating for varicoceles.
Anatomy
The testicles and associated structures are located within the scrotum, formed by fusion of three fascial layers and divided by a median septum. 1 The septum is contiguous with the dartos muscle underneath the scrotal skin. The tunica vaginalis is a potential space formed from the processus vaginalis, an outpouching of the fetal peritoneum that descends into the scrotum along with the testis. An inner visceral layer covers the testis and epididymis, and an outer parietal layer lines the scrotum. The layers join at the posterolateral aspect of the testis where it attaches to the scrotal wall. The tunica albuginea forms a dense capsule around the testis, and a reflection of this capsule along the posterior border (the mediastinum testis) runs along the superior inferior axis of the testis. The mediastinum divides the testis into lobules and serves as a conduit through which the blood vessels, lymphatics, and spermatic tubules enter and leave the testis. The epididymal head is located superior to the testis, while the body and tail run posterior to the testis. The efferent ducts converge and, from the epididymal tail, become a single vas deferens, which continues in the spermatic cord. The spermatic cord also contains the testicular, cremasteric, and deferential arteries, pampiniform plexus, nerves, and lymphatics. 1-3 Four testicular appendages, remnants of embryonic ducts, include the appendix testis, appendix epididymis, vas aberrans, and the paradidymis; 92% of males have an appendix testis, and 34% have an appendix epididymis. 4
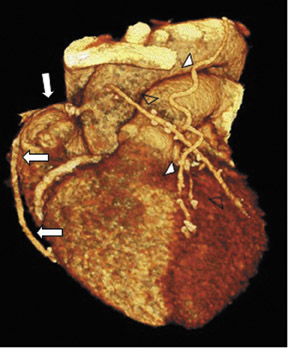
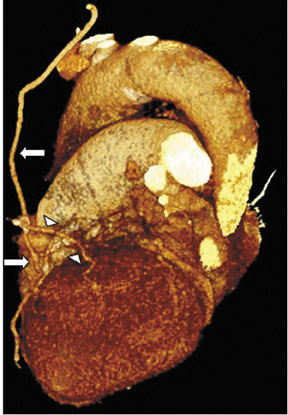
The main blood flow to the testicle is via the testicular artery, with branches off the deferential and cremasteric arteries. These arteries course through the spermatic cord, along with their corresponding veins and nerves. The testicular artery pierces the tunica albuginea, forming capsular arteries that, in turn, form recurrent rami that course centrifugally toward the mediastinum. In 10% to 50% of normal testes, a single transmediastinal artery can be seen unilaterally running directly within the mediastinum and coursing in an opposite direction from the recurrent rami. 1,2,5
Sonography
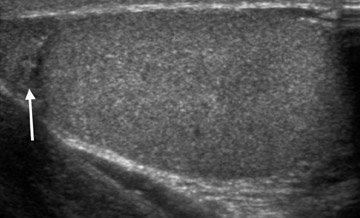
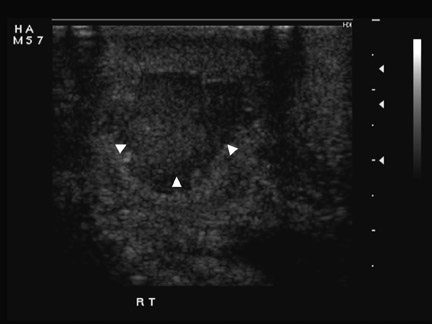
On US, the pediatric testes are ovoid, measuring approximately 1 cm 3 with uniform low-to-medium echogenicity (Figure 1). The size and echogenicity increases from age 8 to puberty, at which time the testes are about 4 cm 3 . In the adult, the normal testis is roughly 20 cm 3 , with an approximate diameter of 3 to 5 cm, which decreases with age. 4 The mediastinum testis can be seen as a linear echogenic band. The trans-mediastinal artery, if present, appears as a prominent intratesticular hypoechoic band with opposite direction of flow from the recurrent rami (Figure 2). The epididymis has an echogenicity similar to or slightly hyperechoic to the testis. The epididymal head may be round or triangular, measures 5 to 12 mm in length, and lies atop the superior pole of the testis (see Figure 1), while the body and tail run posterior to the testis. The narrow body (2 to 4 mm) and tail (2 to 5 mm) are often indistinguishable from surrounding tissues but may occasionally be seen in normal patients with high-resolution US. 2,4 A small amount of fluid between the leaves of the tunica vaginalis is seen in most normal patients. The appendix testis is attached to the upper pole of the testis in the groove between the testis and the epididymis, while the appendix epididymis is attached to the head of the epididymis. These structures are seen only when torsed or when a hydrocele is present 2-4 (Figure 3). The normal scrotal skin measures 2 to 8 mm in thickness. 6
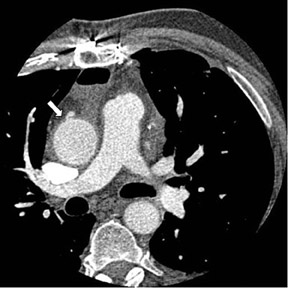
Testicular torsion
Torsion occurs most frequently in adolescent boys with an incidence of 1 in 160 by age 25. Two thirds of cases occur between 12 and 18 years of age. 5 Up to 70% of young boys with acute scrotal symptoms have conditions other than torsion-most commonly epididymitis. Ultrasound is helpful to differentiate testicular torsion from other causes of acute scrotal pain and to identify testicular torsion promptly, ensuring the highest salvage rate. The severity of torsion of the testis can range from 180˚to 720˚, but complete occlusion of blood flow does not occur until 450˚of tor-sion. 4 Transient or intermittent torsion with spontaneous resolution sometimes occurs. Venous congestion progresses to arterial occlusion, testicular ischemia, and infarction. The collateral blood flow is typically not adequate to provide viability to the testicle if the testicular artery is occlud-ed. 5
Testicular torsion can be classified as extravaginal or intravaginal. Extravaginal torsion occurs in utero or perinatally before the testis is fixed, so the torsion occurs proximal to attachment of the tunica vaginalis, in the inguinal canal or just below it. 5 This form of torsion is found exclusively in newborn infants. Intravaginal torsion is more common and is due to a bell-and-clapper deformity in which the tunica vaginalis has an abnormally high insertion on the spermatic cord and completely encircles the testis, leaving the testis free to rotate within the tunica vagi-nalis. 3,5 The deformity is bilateral in most cases. 4 Intravaginal torsion may also occur in testes that are retractile or are not fully descended. Blunt trauma, sudden forceful rotation of the body, or sudden exertion also predispose to testicular torsion.
The sonographic appearance of testicular torsion depends on the duration of the torsion. Within 6 hours, the affected testis may be slightly enlarged, with normal or decreased echogenicity (Figure 4A). After 24 hours (late or missed torsion), echogenicity of the testis becomes heterogeneous, a sign of loss of viability. 3,5 The epididymal head may be enlarged because of involvement of the deferential artery. Hydroceles are common. 4,7 Spiral twisting of the spermatic cord may be seen with color Doppler imaging. Normal testicular echogenicity and lack of scrotal wall thickening or hydrocele are strong predictors of testicular viability. 4 Color Doppler imaging provides both structural and physiologic information about the vascular integrity of the testis. Doppler flow may be difficult to demonstrate in young children, even within the normal testis. 3 Unilateral diminished or absent flow is the most accurate sign of testicular torsion (Figure 4B), but the presence of blood flow does not exclude torsion. 7 False-negative studies may occur when torsion is intermittent or low grade. The torsion may result in hyperemia, mimicking epididymo-orchitis. Late torsion may be accompanied by peripheral blood flow, but central testicular blood flow will be absent. Intravenous microbubble contrast material may improve US sensitivity but is not routinely available. There are a few advocates of manual detorsion of the twisted testis under narcotic analgesia, but it is yet unclear whether this maneuver increases the salvage rate in torsion.
Torsion of the testicular appendages occurs less frequently than does testicular torsion (6:1) but can be as painful. Sonography is important for distinguishing this condition, which is self-limiting and does not threaten testicular viability. Clinically, the cremasteric reflex is preserved and a palpable nodule with bluish discoloration (blue dot) is often detected. Approximately 91% to 95% of cases involve the appendix testis in boys 7 to 14 years of age.Ultrasound shows a hyperechoic mass with central hypoechoic area adjacent to the testis or epididymis. Other associated findings include scrotal wall edema and epididymal enlargement. Blood flow in the peritesticular structures may be increased. Ultrasound is helpful to exclude testicular torsion, because blood flow within the testis is normal in torsion of the appendix testis. Torsed appendages may atrophy and calcify. 4 Occasionally, in infants, calcified meconium from an in utero intestinal perforation can descend into the scrotum, mimicking the hard mass of an infarcted testis. Segmental testicular infarction can occur in the absence of torsion, resulting from trauma, vasculitis (Figure 5), or tumor.
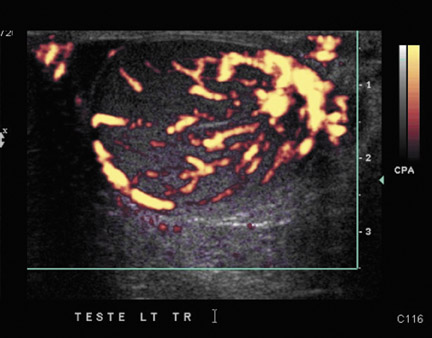
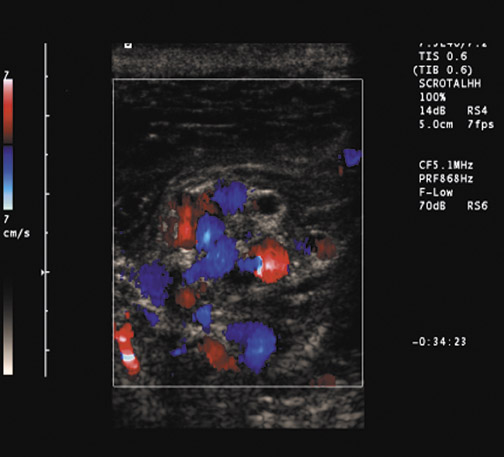
Inflammation
Inflammatory causes of scrotal pain predominate in all age groups. Epididymitis usually results from descending infection, frequently associated with urinary tract infection. Genitourinary anomalies (such as ectopic ureter, ectopic vas deferens, or urethral stricture) may predispose a child to epididymitis. In pubertal boys and young adults, epididymitis most commonly results from sexually transmitted diseases. Less commonly, epididymitis may result from hematogenous infection, trauma, idiopathic granulomatous disease, and vasculitides, such as Henoch-Schönlein purpura and Kawasaki disease. Chemical epididymitis from amiodarone hydrochloride, an antiarrhythmic agent, has been described. 5 With infectious epididymitis, the process begins in the tail and proceeds cephalad. On US, the epididymis is enlarged and hypoechoic or heterogeneous in echotexture 7 (Figure 6). Often there is a reactive hydrocele and scrotal wall thickening. Associated orchitis is seen in 20% of cases and may be diffuse or focal, characteristically seen as a crescentic hypoechoic lesion within the testicle, located at the periphery near the inflamed epididymis. 1 Isolated orchitis is rare, and is usually a result of postviral or posttraumatic inflammation (Figure 7). On color Doppler, epididymitis is seen as diffuse or focal areas of increased color signal (Figure 6B). Hyperemia is the only US finding in 20% of patients with epididymitis and 40% of patients with orchitis. 3,7 Focal hyperemic areas may mimic testicular mass, hypervascular epididymal tumors, or spontaneous detorsion of testis with hyperemia. 5,7 Testicular ischemia may occur secondary to venous outflow obstruction. 3,4 Fournier's gangrene is a polymicrobial necrotizing fasciitis of the scrotum that can extend to the lower abdominal wall. 4 The diagnosis of Fournier's gangrene is made when soft tissue air is seen as echogenic foci with shadowing within the scrotal tissues. Such air can be differentiated from bowel within an inguinal hernia by demonstration of peristalsis of intestinal loops. The scrotal skin is usually thickened and hyperemic in scrotal fasciitis. Other complications of epididymitis include infarction, abscess, and pyocele formation. 5,7 Idiopathic scrotal edema can occur in boys 4 to 7 years of age. The scrotal skin is edematous, but the testis and epididymis are normal. 3
Hydrocele
In most normal patients, a small amount of fluid (1 to 2 mL) can be seen within the leaves of the tunica vaginalis. 2 Hydrocele is present when an excessive amount of fluid is present. 4 Hydrocele is the most common cause of painless scrotal swelling and may develop secondary to trauma, infection, testicular torsion, or tumor. Idiopathic hydroceles also occur. Congenital hydrocele results from a patent processus vaginalis that allows ascites to enter the scrotal sac. When the fluid contains high protein or cholesterol content, the hydrocele may appear complex or septated. 6 Hematoceles and pyoceles are rare and are usually caused by trauma, surgery, or neoplasm. Pyocele from untreated infection or rupture of abscess typically shows internal septations and loculations on US (Figure 8). Skin thickening and calcifications may also be present.
Inguinal hernia
Inguinal hernias occur because of protrusion of peritoneal contents, usually omentum or bowel, through a patent processus vaginalis. Hernias are classified as direct or indirect by their relationship to the inferior epigastric artery (IEA). Direct hernias are located medial to the IEA, while indirect hernias are lateral to the IEA. 8 Fluid or air-filled loops of bowel with peristalsis in the scrotal sac are diagnostic of an inguinal hernia (Figure 9). Hyperechoic areas are likely to represent omentum. Incarceration of a hernia is most common before 6 months of age and in adulthood and is more common in indirect hernias. The presence of an akinetic dilated loop of bowel within the scrotum has a 90% sensitivity and specificity for strangulation. Be wary of contraction of the dartos muscle, which can cause movement that may mimic bowel peristalsis. The bowel wall can be thickened and hyperemic with incarcerated hernias. A Richter hernia consists of herniation of only the antimesenteric border of the bowel and may not result in intestinal obstruction. The diagnosis of Richter hernia is difficult to make sonographically.
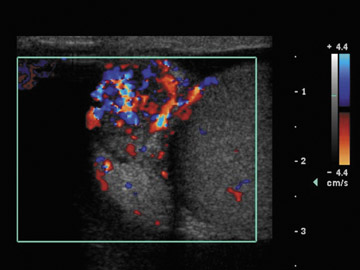
Varicoceles
Varicocele represents abnormal dilatation and tortuosity of the veins of the pampiniform plexus within the spermatic cord, caused by incompetent valves in the internal spermatic vein. The condition is more common on the left and is idiopathic in 15% of males between 15 and 25 years of age. 2 About one third of men with varicocele will be infertile. The size of the varicocele does not affect the incidence of infertility. 9 On US, varicoceles appear as multiple hypoechoic serpiginous and tubular structures of varying sizes, predominantly >2 mm in diameter and located superior and lateral to the testis. 2,4 Echoes from slow blood flow may be seen within the dilated veins (Figure 10). Noncompressibility of a varicocele may indicate retroperitoneal malignancy or other causes of increased pressure on the spermatic vein. Ultrasound with color Doppler is highly sensitive for the diagnosis but requires scanning in both the supine and upright positions and during the Valsalva maneuver. Primary varicoceles may decompress when the patient is supine, but the flow within the veins increases when the patient is in an upright position and with the Valsalva maneuver.
Trauma
The scrotum and its contents are commonly injured during motor vehicle accidents and athletic injuries. Direct blow or straddle injuries result in contusion, hematoma, fracture, or rupture. More than 50% of testicular ruptures occur from a direct blow to the groin during sporting activity. 4 Testicular injuries are surgical emergencies with good prognosis if treated within 72 hours. Ultrasound shows heterogeneous echogenicity within the testis due to areas of hemorrhage or infarction. Other findings include irregular, poorly defined borders, scrotal wall thickening, and hematocele (Figure 11). The tunica is disrupted with testicular rupture, and there may be diminished blood flow in the disrupted capsule. A large hematocele may displace and obscure the underlying testis, leading to a false-positive diagnosis of testicular rupture. 7 In testicular fracture without rupture, the capsule is intact but a discrete fracture plane is visible in only 17% of cases 7,10 (Figure 12). It is important to remember that 10% to 15% of tumors first manifest after trauma and can mimic an injury; therefore, sonographic abnormalities should be followed to resolution if surgery is not performed. 11
Tumors
Testicular and paratesticular tumors can occur in all age groups but are an uncommon cause of acute scrotal pain (10%). 5 Testicular tumors are more likely malignant, while extratesticular tumors are more likely benign. In general, palpable masses are more likely to be malignant than are nonpalpable masses. 4 The role of US is to distinguish intratesticular from extratesticular lesions. Approximately 90% to 95% of testicular tumors are germ cell tumors, most commonly seminomas. Nonseminomatous germ cell tumors are usually of mixed cell types. Other testicular tumors include gonadal stromal tumors, lymphoma, leukemia, and metastases. 2 The differential diagnosis of focal testicular mass includes hematoma, abscess, focal orchitis, infarction, and granulomatous disease. Color Doppler imaging can help to differentiate such abnormalities from tumor, but distinction may be difficult when tumor presents as generalized testicular enlargement without focal mass. In up to 15% of patients, signs and symptoms caused by metastatic disease are the first indication of testicular tumor. Occasionally, the primary tumor may have undergone spontaneous regression and appear as an irregular scar or calcification without a definite mass. 6
The adenomatoid tumor of the epididymis is the most common extratesticular tumor in adults. Adenomatoid tumor is a benign hamartoma that favors the epididymal tail. 11 Other extratesticular tumors include lipomas, leiomyomas, lymphangiomas, sarcomas, and metastases. Malignant lesions to the scrotal wall are usually of epididymal origin. The most common malignant paratesticular tumor in infants and children is rhabdomyosarcoma, which is associated with a better prognosis than rhabdomyosarcoma found elsewhere in the genitourinary tract.
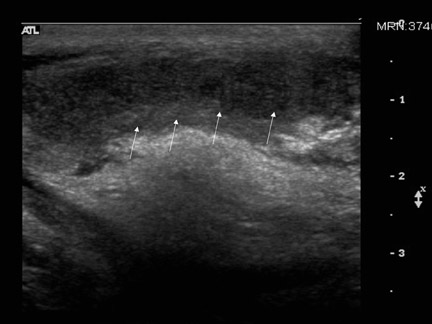
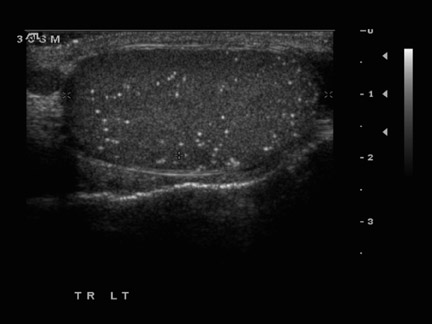
Testicular microlithiasis (TM) is defined as multiple (>5) echogenic nonshadowing 2- to 3-mm foci randomly scattered throughout the testicular parenchyma (Figure 13). The number, distribution, and laterality of the foci varies. Diagnosis requires high-frequency US transducers. 12 Testicular microlithiasis is associated with cryptorchidism, infertility, pulmonary alveolar microlithiasis, and intratubular germ cell neoplasia. Eighteen percent to 75% of patients are at risk for testicular cancer, primarily nonseminomas. 4 The relation of the number of calcifications to cancer risk has not been well established, but in the absence of a focal mass, annual follow-up is recommended in all patients with TM. 12 Fibrous septae in normal testes can mimic the foci of TM, but normal septae disappear when scanned at a 90° angle.
Miscellaneous scrotal abnormalities
Epididymal cysts and spermatoceles are common at all ages. Both types of lesions can be multiple, and about 30% of cases are asymptomatic. 6 Both types of cysts are thought to result from dilatation of the epididymal tubules. Epididymal cysts contain clear serous fluid, and spermatoceles generally contain spermatozoa and cellular debris. The sonographic appearance of these cysts is similar; however, epididymal cysts can occur anywhere, while spermatoceles occur only in the epididymal head. 4 Tubular ectasia of the rete testis can present as multiple cystic lesions, but its characteristic location near the mediastinum testis should prompt the diagnosis. Benign testicular cysts include tunical albuginea cysts, testicular cysts, and epidermoids (keratocysts). 2
An undescended testis is one of the most common genitourinary anomalies in male infants. Cryptorchidism is found in 3.5% of term male infants at birth. Cryptorchidism is usually unilateral, but up to 30% of cases are bilateral. Associated urologic anomalies can be seen in up to 20% of patients with an undescended testis. The undescended testis is most commonly located at or just below the inguinal canal (Figure 14). Patients with an undescended testis are at higher risk for malignancy, torsion, infertility, and incarcerated inguinal hernia. 4 The risk of death from testicular malignancy in men with an undescended testis is nearly 10 times the risk in normal men, and the risk is increased in both the undescended testis after orchiopexy and within the normally descended testis. 2
Macroscopic calcifications within the scrotum can be intratesticular or extratesticular. Intratesticular macrocalcifications may be associated with large cell calcifying Sertoli cell tumor, burned-out germ cell tumor, 6 or dystrophic calcifications from prior trauma. 4 In the epididymis, macrocalcifications may be the result of inflammation or trauma. Scrotoliths (scrotal pearls)-calcified bodies within the scrotum with no clinical importance-may represent loose bodies caused by torsion of the appendix testis or epididymis 4 (Figure 15).
Conclusion
High-resolution US is the imaging modality of choice in the evaluation of the acute scrotum. Knowledge of the normal appearance of the testis and scrotal contents and familiarity with the many pathologic conditions that may affect the scrotum are essential for expedient and accurate diagnosis of scrotal pathology. Proper US technique is critical, especially in the evaluation of torsion and testicular rupture. Some conditions have overlapping sonographic features, and follow-up to resolution is required to exclude underlying malignancy.
Related Articles
Citation
Ultrasound of the acute scrotum. Appl Radiol.
March 6, 2006