Thoracic imaging in the intensive care unit
Images








Dr. Fishman is an Associate Professor of Radiology, University of Miami School of Medicine, and Director of Diagnostic Radiology, Jackson Memorial Hospital, Miami, FL. Dr. Primack is a Professor of Radiology and Medicine and Vice Chairman, Department of Radiology, Oregon Health and Science University, Portland, OR.
Although this material has not been published in manuscript form, some of the material has been presented in part at the following meetings: "Critical Care Radiology," American Thoracic Society Annual Meeting, Atlanta, GA, May 2002; "Thoracic ICU Radiology," Society of Thoracic Radiology Annual Meeting, Miami Beach, FL, March 2003; "Chest Imaging in the Intensive Care Unit," University of Miami Symposium: Imaging, Intervention, and Innovation, Miami
Physical examination is often difficult in the intensive care unit (ICU) setting and for many years has been complemented by the portable chest radiograph (CXR). The interpretation of portable ICU radiographs may also be difficult because of the limitations of applying optimal radiographic technique in the ICU setting, as well as the patient's condition and the presence of monitoring and other devices (either in or on the patient) that might obscure portions of the chest. Studies have shown a wide range of utility of these radiographs, and, to date, there have been only limited studies claiming to document cost-effectiveness. 1,2 According to some studies, 43% to 65% of all ICU CXR had "unexpected or ab-normal findings," 3-7 many of which affected management. If limited to a "routine" daily CXR, efficacy decreased to 15% to 18% in a medical or respiratory ICU setting and decreased even further (5%) in the cardiothoracic ICU. In pediatric ICUs, 45% of daily radiographs led to interventions being performed; smaller, more critically ill children with one or more life- support devices were the most common patients to undergo such interven-tions. 8
The American College of Radiology has addressed these issues in its Appropriateness Criteria, 9 stating that a daily CXR is indicated for patients with acute cardiopulmonary problems and for patients on mechanical ventilation. In patients with a central venous catheter, a Swan-Ganz catheter, a feeding tube, or a chest tube placement, only postprocedure radiographs are indicated. Stable cardiac monitoring patients and those with purely extrathoracic disease require only admission films upon entry into the ICU.
Cardiopulmonary disorders
Atelectasis
Atelectasis is the most common cause of lung opacity in an ICU patient. There is an increased incidence after general anesthesia and thoracic/upper abdominal surgery. The incidence is also increased in patients with pre-existing lung disease, smokers, obese patients, and the elderly. The left lower lobe is the most common location. In many cases, the atelectasis is linear or plate-like. However, atelectasis may be patchy and may mimic pneumonia. In recumbent patients, radiographic evidence of volume loss may not be evident and differentiation of atelectasis from consolidation can be difficult. In lobar atelectasis, the presence or absence of air bronchograms is useful to determine the potential effectiveness of therapeutic bronchoscopy. 10 If air bronchograms are present, the atelectasis is most likely related to the collapse of small airways, and bronchoscopy likely will not be therapeutic. However, if air bronchograms are absent in lobar atelectasis, mucoid impaction is the most likely etiology and therapeutic bronchoscopy has a high likelihood of being beneficial (Figure 1).
Edema
Pulmonary edema is one of the most common abnormalities affecting ICU patients. Causes of edema are broadly grouped into 2 categories: 1) hydrostatic edema, including heart failure, overhydration, and renal failure; 2) permeability edema, including adult respiratory distress syndrome (ARDS), sepsis, drug reaction or allergy, near drowning, smoke or toxic fume inhalation, neurogenic edema, aspiration, fat embolism, and others.
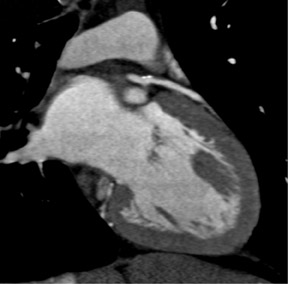
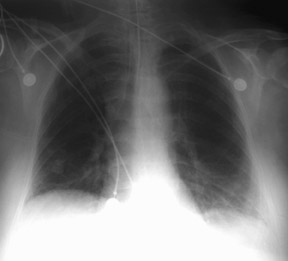
The first radiographic sign of hydrostatic imbalance is engorgement of the pulmonary veins, reflecting an elevation in left ventricular end-diastolic pressure (LVEDP). Cephalization of the vasculature is not very helpful in the ICU setting because many films are obtained in the supine position, which redistributes vascular volumes. Nevertheless, a study of 135 supine ICU patients found that pulmonary wedge pressures >18 mm Hg could be detected by a vascular pedicle (mediastinal width at the superior vena cava [SVC]) measuring ≥70 mm and a cardiothoracic ratio (the width of the heart to the width of the lungs at the bases) of ≥55%, yielding a 70% accuracy. 11 These results were better than subjective interpretation of the films without (56%) or with (65%) clinical data. The true edema phase is first characterized by interstitial fluid, manifested by indistinct vessel margins, thickening of bronchi, Kerley lines (A, B, or C), hazy or "ground-glass" opacities, and a gravity-dependent increase in density (particularly on CT scans). Pleural effusions begin to accumulate as interstitial fluid overloads the venules and lymphatics of the interstitium. Effusions may be bilateral or only right-sided; a solely left-sided effusion suggests a superimposed process (or gravity). Interstitial edema is radiographically indistinguishable from infections, such as pneumocystis and cytomegalovirus pneumonias, but daily changes are suggestive of edema rather than infection. Edema with the highest LVEDP manifests as alveolar opacification, typically bilateral and reasonably symmetric. However, there are many reasons for asymmetric edema, including gravity (eg, bedridden, immobile patients), underlying lung disease that alters blood flow (eg, chronic obstructive pulmonary disease, fibrosis), cardiac disease (eg, mitral regurgitation) (Figure 2), pulmonary vascular disease (eg, shunts, pulmonary embolism, hypoplastic vessels), and re-expansion after thoracentesis or pneumothorax evacuation (Figure 3). Alveolar edema may be indistinguishable from hemorrhage or diffuse pneumonia. After cardiac surgery, patients generally exhibit at least mild edema, but they typically improve daily.
Permeability edema (often called noncardiogenic) lacks the pulmonary venous engorgement noted above. An advanced form of permeability edema, ARDS, is defined by decreased lung compliance, normal LVEDP, and hypoxia refractory to O 2 . Initially, there may be no abnormalities on the CXR (up to 12 hours postinsult). Subsequently, the radiograph shows a pattern of edema (at 12 to 24 hours), which is usually patchy, although it can progress to diffuse disease (36 to 72 hours). Air bronchograms are characteristic (89%) 12 and help distinguish ARDS from hydrostatic edema (Figure 4). Additionally, Aberle et al 13 found that 87% of hydrostatic and 60% of permeability edema could be correctly identified, with a patchy peripheral distribution seen in 58% with permeability edema but only 13% with hydrostatic edema. Decreased lung volumes are frequently observed. Pleural effusions, if present, are usually small. Radiographic findings of barotrauma are common (see below). Adult respiratory distress syndrome progresses from an exudative to an organizing phase, which can lead to a pattern of interstitial fibrosis that may be fixed or may resolve slowly.
Aspiration
Aspiration is very common in ICU patients. Aspiration and its consequences can be divided into 3 forms: Aspiration pneumonitis, aspiration pneumonia, and obstruction of a central airway. The severity of aspiration is related to the volume and type of the aspirate. Factors that increase the risk of aspiration in an ICU patient include general anesthesia, depressed consciousness, neuromuscular disorders, esophageal disease, and the presence of a nasogastric (NG) tube or an endotracheal tube. Focal or multifocal consolidation in a dependent location is the most common radiographic finding. 14 Poorly defined nodules in an airway distribution resulting from acinar filling are often identified (Figure 5). Airway thickening and plugging, as well as associated volume loss, are also commonly identified. Aspiration pneumonitis may progress over the first day but should show clearing within the first few days. A lack of clearing or progression is suggestive of the development of pneumonia. In the recumbent patient, the aspiration is typically located in the posterior aspects of the upper lobes, the superior segments of the lower lobes, and the posterior basilar segments of the lower lobes. This distribution results in a central predominance on the anteroposterior (AP) supine radiograph.
Pneumonia
Most pneumonia in the ICU are due to either mixed anaerobic or aerobic gram-negative organisms. They are commonly related to aspiration. Opportunistic infection should be considered if the patient is immunosuppressed. The incidence of pneumonia in the ICU is approximately 10%; however, in patients with ARDS, the incidence has been reported to range from 20% to 60%, with a 70% incidence at autopsy. 15 Although pneumonia is commonly present in patients with ARDS, the CXR radiograph is only 30% to 50% accurate. 15 The CXR typically shows patchy areas of consolidation or poorly defined opacities that are often multifocal (Figure 6). Air bronchograms are helpful in the diagnosis of pneumonia, but they may also occur in areas of atelectasis. When present, cavitation is a more specific finding of pneumonia. Radiographic changes in pneumonia typically occur more slowly than in atelectasis, aspiration, or pulmonary edema.
Barotrauma
An estimated 4% to 15% of patients on ventilators develop barotrauma, manifesting as abnormal air collections in the chest. 16,17 Underlying lung disease, such as pneumonia and especially ARDS, raise the risk significantly. The effects of barotrauma are generally more severe in children and adults up to age 40. The major factors associated with development of barotrauma include a peak inspiratory pressure >40 cm H 2 O, the use of positive end-expiratory pressure (PEEP), and an inappropriately large tidal volume. Positive pressure ventilation affects the CXR in a number of ways. The CXR visually improves with PEEP and "sighs," especially in edema. Positive end-expiratory pressure improves aeration mostly in the nondependent lung; a mildly abnormal lung fares better than do dense consolidations and dependent regions. The heart size decreases, as does the cardiac output. Pulmonary vessels may decrease or increase in size. Interstitial pulmonary edema has a protective effect against barotrauma because of the elevated interstitial pressures.
The initial abnormal air collection in barotrauma is pulmonary interstitial emphysema (PIE), most often identified in children. Streaky lucencies radiate from the hila, without branching or tapering as do air bronchograms. The gas collections can grow into bubbles, clefts, and cysts between 1 and 8 cm in size. Cysts may resolve or persist and can become superinfected. Patients with ARDS frequently develop cysts at the lung bases. Pulmonary interstitial emphysema carries a significant risk of pneumothorax (77%) from rupture of a cyst. 18 The risk of PIE spreading to the mediastinum is 37%.
Pneumothorax (PTX) is the most concerning sequela of barotrauma. It occurs in up to 25% of ventilated patients, and the risk increases with increased time on the ventilator. Pneumothorax is often associated with, but not caused by, pneumomediastinum. In the supine patient, PTX is usually anteromedial or subpulmonic (lucent upper quadrants of the abdomen, sharp superior surface of the diaphragm, deep sulcus sign, and visualization of the inferior surface of consolidated lung). Less often, the PTX is apical, lateral (displaces the minor fissure from the chest wall), or posteromedial. If PTX is suspected but not definite on supine CXR, then upright, expiratory, or bilateral decubitus radiographs should be obtained (Figure 7). False-positive appearances of PTX may be due to skin folds, overlying tubing/dressing/lines, and prior chest tube tracks. The size of the PTX is unrelated to its significance, since even a tiny PTX can acutely enlarge in ventilated patients. Tension is present in 60% to 96% of ventilated PTX cases 19,20 and signifies that pleural pressure exceeds atmospheric pressure. Mediastinal shift is not always present in tension PTX, possibly masked by PEEP. Signs of tension include displacement of the anterior junction line, azygoesophageal recess, and flattening of heart and vascular shadows. 21
Pneumomediastinum is important as a general sign of barotrauma and must be distinguished from a PTX. Except in rare cases of tension, pneumomediastinum is not a life-threatening condition. Pneumothorax, pneumopericardium, and the Mach effect all mimic pneumomediastinum. Pneumomediastinum may show air streaking into the neck, a "continuous diaphragm," and/or retroperitoneal air. Other manifestations of barotrauma include subcutaneous air and pneumopericardium.
Pleural effusion
Pleural effusions are common in patients in the ICU. The supine CXR shows only moderate (67%) accuracy for identifying effusion, 22 which is improved on lateral and decubitus films. What appears to represent pleural effusion on a portable upright film may, in fact, represent atelectasis (Figure 8). 23 Pleural effusion is difficult to characterize on plain films, except in certain settings. Sudden large effusions suggest hemothorax in a postprocedure patient. Empyema may appear as a loculated (nonmobile) effusion in a patient with fever. After cardiac surgery, effusions are common, particularly as pulmonary edema moves into the pleural space. However, increasing effusion past the third postoperative day may signal a postpericardiotomy syndrome, especially if pericardial effusion and pulmonary opacity are present.
Monitoring and support devices
Endotracheal and tracheostomy tubes
The tip of the endotracheal tube should ideally be 4 to 6 cm above the carina with the neck in a neutral position. If the neck is flexed, the tube can migrate up to 2 cm inferiorly, while extension of the neck can cause migration of the tube up to 2 cm superiorly. If the endotracheal tube is advanced too far, it will typically extend into the right main bronchus (Figure 9). The balloon should be assessed to ensure that it is not overinflated. The balloon should not be greater than the diameter of the trachea. A ratio of the cuff to tracheal lumen >1.5 leads to an increased risk of tracheal damage. Aspiration can occur in up to 8% of patients with endotracheal tubes. Other complications of endotracheal tube placement include dislodging of teeth or fillings, tracheal rupture, and tracheal stenosis, as a chronic complication. 24
Flexion and extension of the neck do not affect the position of a tracheostomy tube. The tip of the tracheostomy tube should be at approximately the T3 level. The balloon should not distend the tracheal wall and the lumen of the tracheostomy tube should be approximately two thirds of the tracheal diameter.
Feeding and nasogastric tubes
The most important consideration is to ensure that NG tubes, especially those through which feeding occurs, are positioned in the stomach or distally and not within the respiratory tree. Often, a patient will have both suction and feeding tubes, and a request to "check NG tube placement" should prompt a search for both types of tubes.
Cardiovascular catheters and other intravascular devices
The tip of a central venous catheter should be between the right atrium and most proximal venous valves. The proximal venous valves are approximately
2.5 cm distal to the junction of where the subclavian and jugular veinsmeet to form the brachiocephalic vein. Therefore, a central venous catheter tip should be medial to the first anterior rib or beyond. Aberrant placement of central venous catheters include placement into normal smaller branch veins or anomalous veins, such as a persistent left SVC. Other important complications include intra-arterial or extravascular placement (Figure 10). The radiograph should also be assessed for the presence of a pneumothorax or hemothorax.
Pulmonary artery catheters (Swan-Ganz catheters) measure pulmonary artery and capillary wedge pressures. The tip should be in the main right or left pulmonary artery and should not be distal to the proximal interlobar pulmonary artery. Approximately 24% of these catheters are malpositioned on the initial CXR and need to be repositioned. 25 Complications include pulmonary infarction, pulmonary artery rupture, cardiac perforation, intracardiac knots, and arrhythmias.
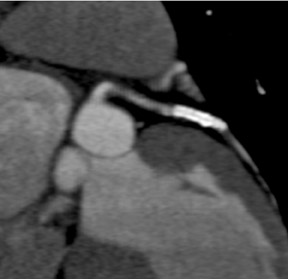
Intra-aortic balloon pumps (IABP) are used for the treatment of cardiogenic shock. These devices increase coronary perfusion and decrease cardiac afterload. The balloon deflates in systole and inflates in diastole, when it may occasionally be seen as a tubular lucency on the radiograph. The tip should be just distal to the left subclavian artery in the proximal descending aorta, approximately 1 to 2 cm below the top of the aortic arch. 26 Too proximal or too distal positioning may lead to complications.
Chest CT in the ICU
CT scanning is increasingly being used in critically ill patients who may have multiple medical problems that may not be easily discriminated by the CXR. It has been estimated that 24% to 75% of ICU chest CTs show "clinically useful" information, 27 translating to a change in management in 22% to 39% of scanned cases. 28,29 However, there remains the risk and cost of transporting patients from the ICU to the scanner and back. 30
Major categories in which chest CT has proven useful are:
Pleural disease-- Mirvis et al 31 found that 30% of trauma ICU CT showed significant effusion with possible empyema. Pleural enhancement with contrast suggests an exudative process, such as hemorrhage, empyema, or tumor. Further- more, CT is far superior in quantifying effusions as compared with the CXR.
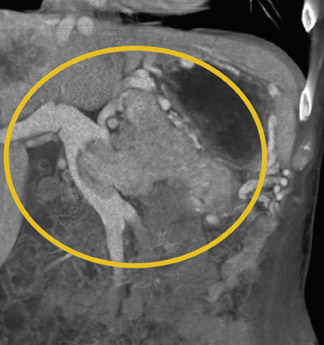
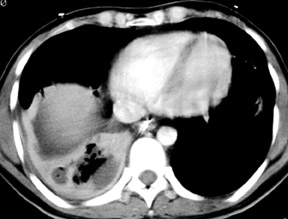
Pulmonary disease-- CT may detect unsuspected pneumonia or tumor. CT is far superior to the CXR for detecting cavitation, and, therefore, can help identify abscess and differentiate it from empyema (Figure 11).
Life support devices-- CT revealed that chest tubes were malpositioned in 15% of cases. 31
Complications of mechanical ventilation -- Although seen on CT, 40% of PTX, 70% of bullae, and 80% of pneumomediastinum were not seen on CXR. 23 Unsuspected PTX was found in 7% of ventilated patients by CT. 31
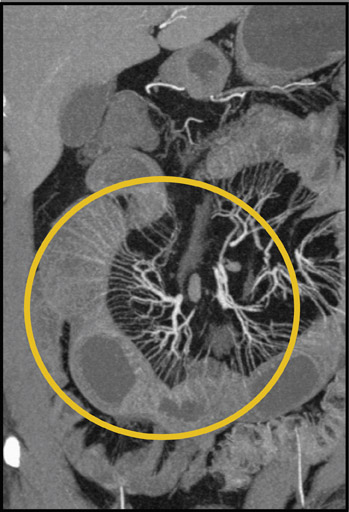
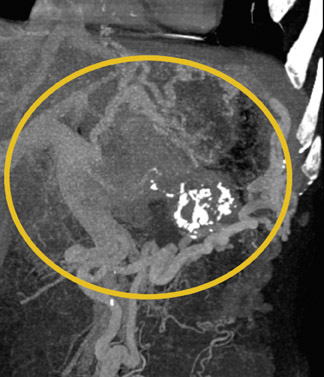
Pulmonary embolism -- Contrast-enhanced CT is becoming a primary test in patients with possible pulmonary embolism, a disease of particular concern in patients experiencing extended hospitalization, such as those in the ICU.
PACS and the ICU
While the installation and integration of a picture archival and communications system (PACS) into daily practice primarily benefits the radiologist in terms of efficiency and workflow, its improved image accessibility and availability allow clinicians, including intensivists, to more easily review the radiographic studies they order. As expected, a study on the presence of PACS workstations in an ICU setting reported decreased time from the radiograph order to actual viewing. 32 In order to maintain or improve the benefit of radiologist input on patient care, timely reporting and/or routine radiologist-intensivist "rounds" or consultation become increasingly important. PACS workstations located within ICU settings are often installed with suboptimal viewing conditions. For example, bright rooms with excessive ambient light and glare may render accurate diagnosis difficult in some instances. Radiologist consultation should be requested when installing new PACS workstations outside of the radiology department in order to optimize the viewing environment, including lighting, ergonomics, and software menu/toolbar layout.
Conclusion
Thoracic imaging, especially using chest radiography, is a crucial component of intensive medical care. Although specific radiographic diagnoses are sometimes difficult to make, the radiograph provides important information about disease progression, and radiographic findings often lead to changes in management. The radiograph is invaluable for verification of life support devices. Computed tomography is particularly useful when radiographic findings are equivocal or are at odds with the clinical scenario.