Radiological Case: Retromandibular vein ectasia
Images






CASE SUMMARIES
Venous ectasias of the retromandibular vein are rare lesions that can mimic a parotid mass on imaging. Here we present 2 such cases and, for comparison, a case of mild widening of the retromandibular vein. A combination of multiplanar imaging and astute clinical examination should lead to the correct diagnosis without surgery.
Case 1
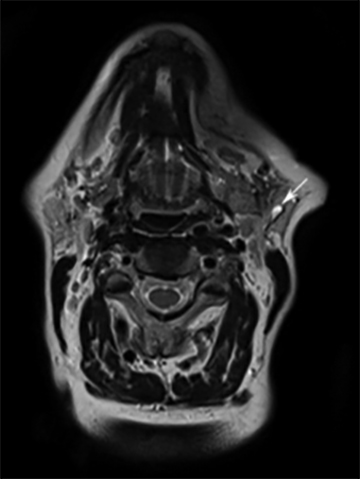
A 69-year-old woman was incidentally noted to have a left parotid mass on a magnetic resonance imaging (MRI) study of the cervical spine. An axial T2-weighted image (Figure 1) from that study showed a well-defined 2-cm left parotid lesion with high signal intensity. Based on the imaging, a diagnosis of a benign or low-grade parotid tumor was suggested, and she was referred to our institution’s head and neck cancer center.
Case 2
A 60-year-old woman initially underwent an ultrasound examination of the lower neck after her primary care physician palpated a neck mass. The ultrasound examination suggested a parathyroid lesion and the patient was referred to our head and neck cancer center, where physicians were unable to palpate a neck mass.
Case 3
A 45-year-old woman had an MRI examination for a thyroid mass.
DIAGNOSES
Cases 1 and 2
Venous ectasias of the retromandibular vein
Case 3
Mild widening of the retromandibular vein
IMAGING FINDINGS
Case 1
A contrast-enhanced computed tomography (CT) scan again showed a well-defined enhancing left parotid mass. Although the mass was round on the axial images, it appeared to be tubular and inseparable from the lower retromandibular vein on the reformatted sagittal images (Figure 1). When the clinicians were consulted, they said they could not palpate a parotid mass in the erect position, but could detect a parotid fullness with the patient supine.
Case 2
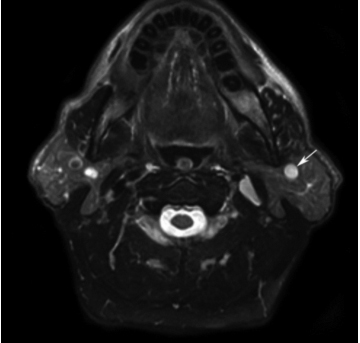
Re-evaluation with an MRI study did not reveal evidence for a parathyroid lesion, but did reveal a left parotid mass. On an axial T2-weightedimage, the mass was well-delineated and had high signal intensity (Figure 2). A T1-weighted, fat-suppressed, contrast-enhanced image showed an enhancing lesion in apparent continuity with the adjacent retromandibular vein (Figure 2). A decision was made to confirm the suspected diagnosis of retromandibular vein ectasia with an MRA and MRV examination of the parotid region. Although there was no interval instrumentation, 5 days later this study showed marked shrinkage of the parotid lesion (Figure 2); however, its relationship to the surrounding vasculature could not be resolved clearly. Similar to Case 1, no mass was clinically palpated with the patient erect, but a parotid fullness was noted when the patient was supine.
Case 3
Incidentally noted on axial, postcontrast,T2-weighted images and sagittal T2-weighted images was moderate, diffuse enlargement of the retromandibular vein (Figure 3). No focal expansion of the vein was noted, and this was considered a normal variant. No mass was clinically palpated with the patient in either the erect or supine position.
DISCUSSION
Venous ectasias in the neck are uncommon, primarily occurring in the internal and external jugular veins.1-3 By comparison, a venous ectasia developing within the parotid portion of the retromandibular vein is rare, with fewer than 10 cases reported in the literature.4-10
The apparent parotid masses seen on routine axial imaging in cases 1 and 2 should have been easily palpated by the clinicians. The fact that these masses were not palpated indicated that they were likely collapsible. This information, combined with the further imaging demonstration of continuity of each mass with the retromandibular vein (also known as the posterior facial vein), confirmed the diagnosis of venous ectasia. Venous ectasias typically are readily noted in the supine, but not in the erect, position; refill when pressure is released in the supine position and may increase in size with a Valsalva maneuver or when the head is lowered beneath the level of the heart.5
Had either mass been an aneurysm of the parotid segment of the external carotid artery, it would have been palpable and likely pulsatile.In addition, such an aneurysm would be present in the erect and supine positions and would not be compressible. Similarly, arteriovenousmal formations in the parotid gland are almost always palpable and often pulsatile.
Although the use of the term “venous aneurysm” appears in the literature, aneurysms today most often are associated with an artery,while ectasia suggests a venous process. Like arterial aneurysms, venous ectasias are caused by structural weaknesses of the vessel wall.This could be the result of local trauma, inflammation, a congenital weakness, localized degenerative changes, and possibly elevated vascular flow and pressure.5 The etiology of retromandibular vein aneurysms are likely similar to those of other venous neck aneurysms and case reports suggest that venous aneurysms of the parotid gland tend to appear suddenly.9,11 One case report found a retromandibular vein aneurysm associated with severe sialadenitis; the authors hypothesized that the associated inflammation may have weakened the wall of the vein.4
The mild diffuse dilatation of the retromandibular vein in Case 3 does not mimic a parotid mass on imaging and is shown to demonstrate the differing imaging appearance relative to the two ectasia cases. Such mild venous enlargement is likely more common than is reported in the literature.
CONCLUSION
Typically, a venous ectasia has no clinical significance other than a cosmetic appearance.8 Rarely, such ectasias can thrombose, cause athrombophlebitis, or even erode the adjacent mandible.7,10 A case of presumed pulmonary embolus from an external jugular vein aneurysm has been reported, and it would seem possible for these to occur in association with retromandibular vein ectasia as well.12
Although definitive diagnosis of a retromandibular vein aneurysm has historically been through surgical excision, our examples show that diagnosis need not await surgery. These cases are presented to illustrate how such parotid venous ectasias can mimic a parotid mass on imaging, and how palpation can resolve an erroneous diagnosis of a parotid mass.
REFERENCES
- Azghari A, Belmir H, Kharroubi A, et al. External jugular vein aneurysm: A rare cause of neck swelling. A report of three patients. J Mal Vasc. 2011;36:395-398.
- Kirmani S, Rashid M, Ali I, Badar F. External jugular vein aneurysm: A rare cause of neck swelling. J Ultrasound Med. 2011;30:1157-1158.
- McCready RA, Bryant MA, Divelbiss JL, Chess BA. Subclavian venous aneurysm: Case report and review of the literature. J Vasc Surg. 2007;45:1080-1082.
- Ilica AT, Senturk S, Kertmen M, et al. Facial vein aneurysm associated with sialadenitis. J Clin Ultrasound. 2012;40:319-321.
- Jensen JL, Reingold IM. Venous aneurysms of the parotid gland. Arch Otolaryngol.1977;103:493-495.
- Manstein ME, Foote J, Manstein CH, Manstein G. Varix of the facial vein. Ann Plast Surg. 1988;21:155-157.
- Poyton H, Arora B. Aneurysm of the Facial Vein: Report of a Case. Oral; Surg Oral Med Oral Pathol. 1970;29:390-393.
- Schulman NH, Carothers A, Gould WJ. Parotid venous ectasia. Am J Otolaryngol. 1981;2:59-61.
- Strome M. Venous aneurysm of the parotid gland: Case report. Ann Otol Rhinol Laryngol.1970;79:1019-1021.
- Wadley JK. Aneurysm of the posterior facial vein. Laryngoscope. 1972;82:821-823.
- Rosenfeld L. Experiences with vascular abnormalities about the parotid gland and upper neck. Arch Surg. 1959;79:553-566.
- Ioannou CV, Kostas T, Tsetis D, Georgakarakos E, Gionis M, Katsamouris AN. External jugular vein aneurysm: A source of thrombotic complications. Int Angiol. 2010;29:284-285.