Radiological Case of the Month(2)





Prepared by Berkeley R. Hanson, MD and Anna K. Henisz, MD, PhD, Department of Diagnostic Imaging and Therapeutics, University of Connecticut Health Center, Farmington, CT, and Paul M. Silverman, MD, M.D. Anderson Cancer Center, Houston, TX.
CASE SUMMARY
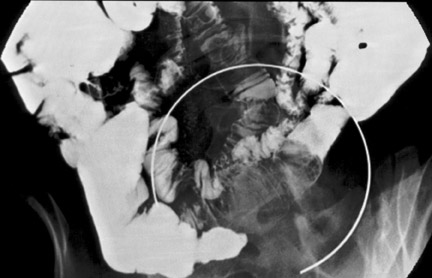
A 60-year-old woman with a history of ventral hernia repair presented with a 1-month history of severe, colicky, periumbilical pain, nausea, and vomiting. Physical examination revealed a soft abdomen with periumbilical tenderness and guarding. Laboratory evaluation was normal. Ultrasound (not shown), computed tomography (CT) (Figure 1), and small-bowel barium study (Figure 2) were performed and followed by laparoscopy.
DIAGNOSIS
Small-bowel lipoma causing intussusception
IMAGING FINDINGS
Ultrasound evaluation of the abdomen showed no evidence of cholecystitis or ascites (not shown). A contrast-enhanced CT of the abdomen and pelvis revealed a well-circumscribed 4-× 4-cm mass of homogenous fatty attenuation within the lumen of the distal small bowel. In the area of the mass, the bowel wall was abnormally thickened and small mesenteric vessels were being pulled into the bowel lumen by an invaginating loop of bowel consistent with a small-bowel intussusception (Figure 1). A subsequent barium small-bowel study showed a filling defect with a coiled-spring appearance in the distal ileum (Figure 2).
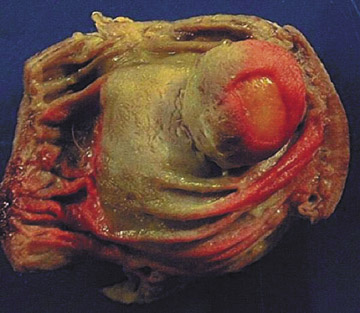
Laparoscopic resection of the involved section of distal ileum was performed. The gross pathologic specimen showed a submucosal lipoma with superficial mucosal necrosis and intense submucosal congestion consistent with intussusception (Figure 3).
DISCUSSION
Historically, lipomas were diagnosed due to small-bowel obstruction, but with the current wide use of CT, especially for evaluation of abdominal pain, CT features are now readily recognized.
Intussusception in adults is relatively rare, occurring in <5% of all intussusceptions and causing approximately 1% of bowel obstructions. 1,2 More than 80% of cases in adults have a known cause, the most common being neoplasm, malignant more common than benign, followed by idiopathic, postoperative complications and adhesions, Meckel's diverticulum, foreign body, inflammation, lymphoid hyperplasia, and celiac disease. Neoplasms serving as the lead point of colonic intussusception are more commonly malignant, while those causing enteric intussusceptions are usually benign. Adult intussusceptions can be ileocolic, colocolic, enteroenteric, or jejunogastric and are without anatomic predilec-tion. 3,4
This case was diagnosed on CT examination and confirmed on a small-bowel barium study. We were able to document intussusceptions on both studies of the same patient. Moreover, the presence of a large ulceration, which was obvious on the pathologic examination, was not visible on either study. Although lipomas are a common benign tumor of the small bowel, second only to leiomyomas, and >50% arise in the ileum, they have rarely been reported as cases of intussusceptions.
Small-bowel lipomas are usually solitary but may be multiple. Most small-bowel lipomas are submucosal and project into the lumen, which can serve as a lead point for intussusceptions. On CT, a lipoma can be identified as a smooth hypoattenuated mass of-50 to -100 HU. 5,6
Antegrade and retrograde barium studies of the small bowel and colon, respectively, can be used to evaluate intussusceptions. In both the small bowel and colon, an intussusception causing incomplete obstruction is found as contrast material trapped between the intussusceptum and intussuscipiens creating a "coiled-spring" appearance. Complete obstruction causes a beak-like appearance at the point of obstruction. 7
Intussusceptions can also be evaluated via ultrasonography, although not typically as an initial study. In cross-section, the alternating layers of mucosa, bowel wall, and mesenteric fat are seen as alternating concentric rings of hyperechoic and hypoechoic soft tissue. 8 Intussusception is best revealed by CT, and its findings are usually pathognomonic. 9
The CT features include a soft-tissue mass with a target-like (cross-sectional images) or sausage-like (sagittal images) appearance. The central area of the target lesion is typically hypoattuenuated, representing invaginated mesenteric fat and vasculature and the intussusceptum, and is surrounded by a thickened intussuscipiens. 10 Other CT findings include trapped oral contrast material between the intussusceptum and intussuscipiens and a thickened bowel wall with intramural air if the vascular supply is compromised. 11
After diagnosis, surgery is required in symptomatic patients or in those who develop related complications. At the time of surgery, the area of intussusception and, if appropriate, the inciting mass are removed. If a benign tumor, such as homogenously fatty mass, is suspected at the time of surgery, a laparoscopic approach should be considered, which is a less invasive procedure; therefore, the patient has a quicker recovery. 12
CONCLUSION
The positive diagnosis of bowel lipoma before surgery will indicate laparoscopic approach rather than a routine laparotomy. This approach is less invasive, is better tolerated, and offers a patient faster recovery.
