Radiological Case: Bronchoesophageal fistula
Images









CASE SUMMARY
A 30-year-old male with a 5-year history of human immunodeficiency virus (HIV) infection, not currently on any treatment, presented to the emergency department (ED) complaining of shortness of breath, and cough aggravated by eating. He had experienced a 30 lb weight loss over the past month, secondary to decreased appetite. Initial labs drawn in the ED were positive for HIV-1 genotype, with a CD4 cell count of 23 (normal >500), and viral load in excess of 175,000 copies (with a goal of “undetectable,” or less than 75 copies).
IMAGING FINDINGS
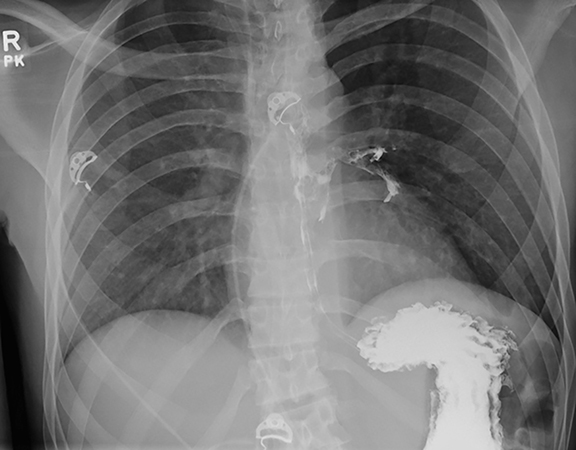
A preliminary chest radiograph obtained in the ED (not shown) revealed a left lower lobe infiltrate. Empiric antimicrobial treatment for aspiration pneumonia was initiated, pending further workup. A modified barium swallow study was performed to evaluate for aspiration. During this exam, no aspiration was witnessed. However, after the patient experienced a coughing fit, contrast was paradoxically observed in the trachea. The study was terminated due to suspicion for a tracheoesophageal abnormality.
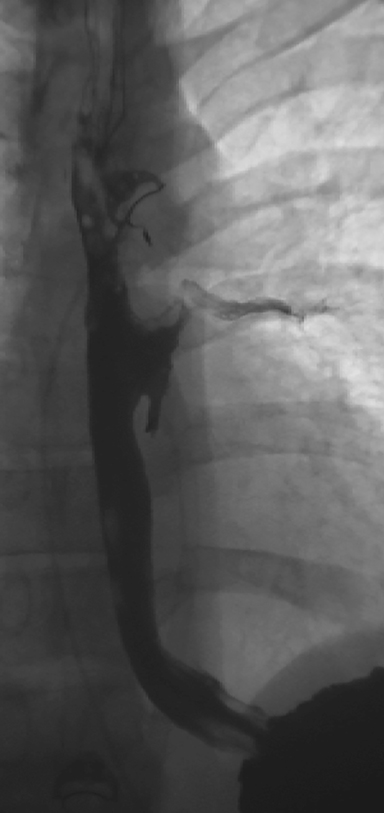
A computed tomography (CT) scan of the neck was obtained. For this particular case, the field of view was extended to just below the level of the carina. It was initially read as negative for any tracheoesophageal abnormality. An esophagram was subsequently performed, and demonstrated a fistulous connection between the esophagus and the left mainstem bronchus (Figures 1 and 2).
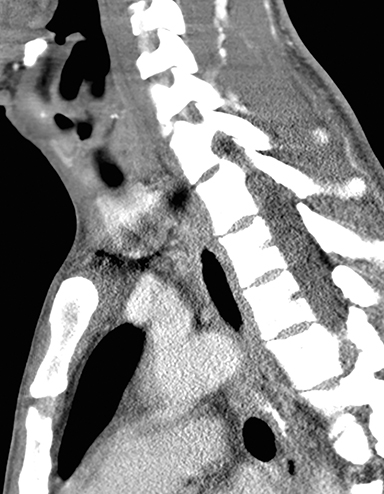
In retrospect, the fistulous connection can be seen on CT, although its appearance is very subtle (Figures 3A-I). Endoscopy was later performed, confirming the presence of a fistula (Figure 4). A biopsy of the esophageal mucosa was obtained; it was negative for cytomegalovirus (CMV) virocytes, but positive for candida species. As candidal colonization of the esophagus is common in HIV-infected individuals with low CD4 counts, candida may be suspected but cannot be proven, as the definitive etiology of bronchoesophageal fistula in our patient.
DIAGNOSIS
Bronchoesophageal fistula
DISCUSSION
An esophagorespiratory fistula (ERF) is an anomalous connection between the esophagus and a portion of the respiratory tract. Tracheoesophageal fistula (TEF) is much more common than bronchoesophageal fistula (BEF). Compared to TEF, few cases of BEF have been reported in the literature.
In the pediatric population, most ERFs are congenital in nature. 1 In adults, malignancy and trauma are by far the two most common etiologies of ERF, respectively.2 It is unusual to see an ERF in an immunocompromised patient, although cases have been documented.3,4 In this clinical setting, ERFs have been reported to result from etiologies such as candida,5,6 CMV,5,6 or a combination of both.7 Mycobacteria (ie, tuberculosis) have also been implicated.8,9 There has even been a report of a TEF in an HIV-infected patient caused by varicella zoster virus.10
Esophagorespiratory fistulas carry a high morbidity and mortality rate, and thus prompt diagnosis and treatment are crucial.1,2 Initial diagnosis is preferentially based on esophagram, although small lesions may be missed.2 The radiologic appearance of an ERF on esophagram is classic, with contrast seen anomalously extravasating into the upper respiratory tract. However, when the suspicion for ERF is high, care must be taken to avoid aspiration, especially in critically ill patients. Endoscopy is the best diagnostic method, as it allows for direct visualization. In this way, biopsies of the mucosa may be obtained, ultimately helping to determine the etiology of the fistula.2
In cases of benign ERF, surgical repair may be performed.4 However, when ERF is secondary to malignancy, palliation is usually the goal, with esophageal stenting being the treatment of choice.2 In the setting of ERF in an immunocompromised patient, though the fistula may be of benign etiology, the patient must be appropriately optimized for surgery to ensure the best possible outcome.2,3
CONCLUSION
Esophagorespiratory fistulas are commonly associated with malignancy or trauma; they are rarely seen in the immunocompromised patient. In the setting of HIV infection, ERF may result secondary to CMV, candida, tuberculosis or even varicella zoster infection. In any patient with findings suspicious for aspiration pneumonia, along with symptoms of coughing, especially when aggravated by eating, radiologists should have a low threshold for suspecting an ERF.
REFERENCES
- Singh J, Olcese VA, D’Amico TA, Wahidi MM. Adult tracheoesophageal fistula: A multidisciplinary approach. Clin Pulm Med. 2008;15:145-152.
- Diddee R, Shaw IH. Acquired tracheo-oesophageal fistula in adults. Contin Educ Anaesth Crit Care Pain. 2006;6(3):105-108.
- Temes RT, Wong RS, Davis M, et al. Esophago- airway fistula in AIDS. Ann Thorac Surg. 1994; 60:440-442.
- Spalding AR, Burney DP, Richie RE. Acquired benign bronchoesophageal fistulas in the adult. Ann Thorac Surg. 1979;28(4):378-383.
- Dieterich DT, Wilcox CM. Diagnosis and treatment of esophageal diseases associated with HIV infection. Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1996;91(11):2265-2269.
- Bartolome S, Klotz S, Bartholomew W. Clinical microbiological case: Esophago-airway fistula in an AIDS patient. Clin Microbiol Infec. 2002;8(3):189-190.
- Rusconi S, Meroni L, Galli M. Tracheoesophageal fistula in an HIV-1-positive man due to dual infection of candida albicans and cytomegalovirus. Chest. 1994;106:284-285.
- Pagano G, Dodi F, Camera M, et al. Tubercular tracheoesophageal fistulas in AIDS patients: Primary repair and no surgery required? AIDS. 2007;21(18):2561-2564.
- Rosario P, Song J, Wittenborn W, Christian F. Tracheoesophageal fistula in AIDS: Stent versus primary repair. AIDS Patient Care STDS. 1996;10(6):334-335.
- Moretti F, Uberti-Foppa C, Quiros-Roldan E, et al. Oesophagobronchial fistula caused by varicella zoster virus in a patient with AIDS: A unique case. J Clin Pathol. 2002;55(5):397-398.