Primary actinomycosis of the breast
Images


CASE SUMMARY
A 48-year-old premenopausal African-American female presented to the emergency room with progressive right breast pain (10/10 severity), erythema and swelling of three days duration. She denied nipple discharge. Four months prior, the patient had right breast mastitis treated with empiric antibiotic therapy, resulting in symptom resolution. Two weeks prior to the current presentation, she had undergone emergent laproscopic cholecystectomy for cholelithiasis and acute cholecystitis. Past medical history was significant for asthma and morbid obesity (BMI 48.6). She reported smoking (two cigarettes per day). Examination of the right breast revealed warm, intact, dry, erythematous skin without rash or drainage from the nipple; the subareolar region was tender and indurated, but fluctuance could not be determined because of patient discomfort. The left breast was unremarkable. Vital signs were within normal limits and white blood cell count was 11,600 WBC/mcL.
IMAGING FINDINGS
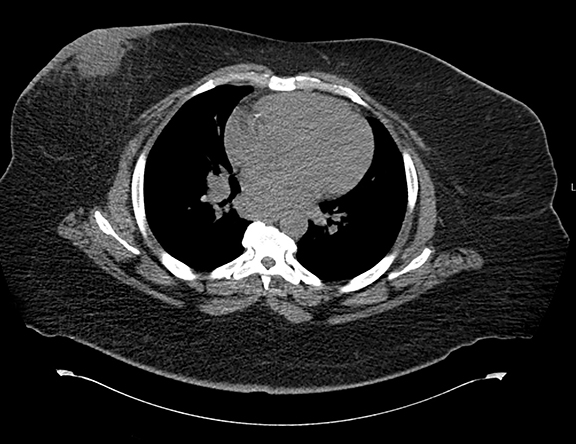
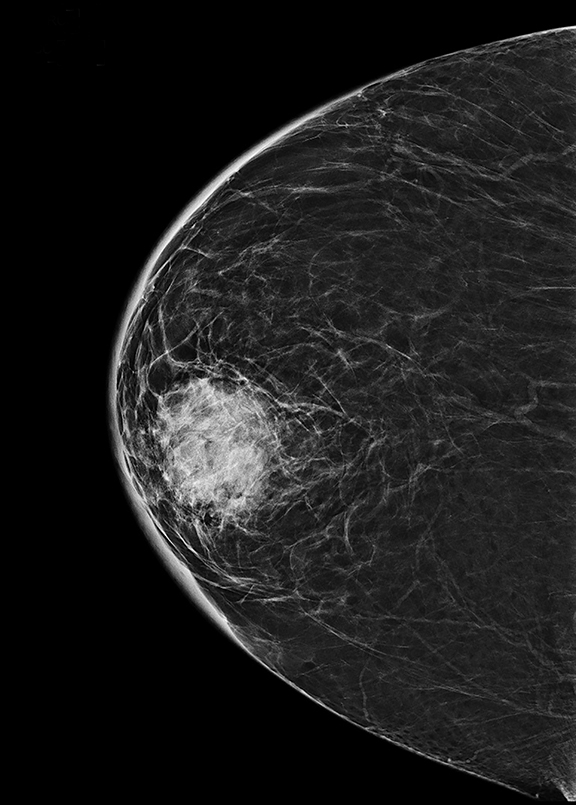
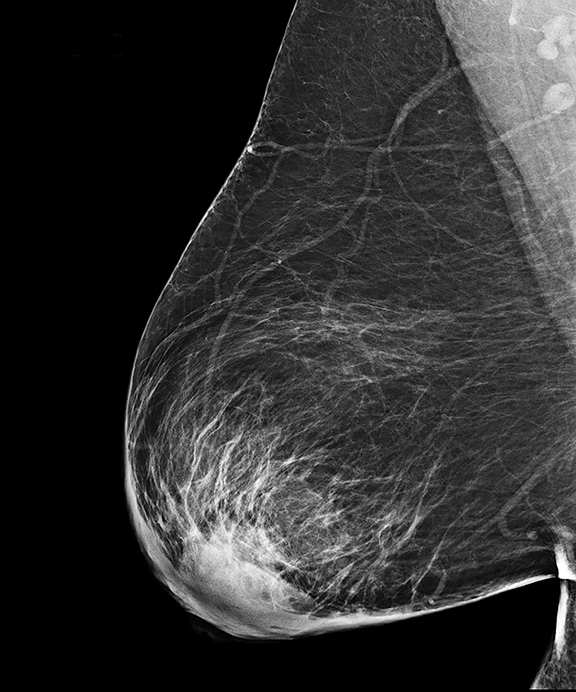
Initial workup included a CT scan of the thorax through the ER, which showed a subareolar mass without central lucency in the right breast, posterior inflammatory stranding, as well as right mediastinal and axillary lymphadenopathy (Figure 1). Further evaluation with a right diagnostic mammogram (standard medio-lateral oblique and cranio-caudal views) revealed a focal asymmetry in the subareolar region (Figure 2), thickening and prominence of the skin in the periareolar location extending up to the middle third of the breast, correlating with the area of redness and swelling on clinical breast examination. Subsequently, targeted ultrasonography of the right breast showed a hypoechoic mass measuring 3.7 × 3.2 × 4.7 cm (Figure 3AB), with increased vascularity surrounding the mass on Doppler interrogation. Skin thickening as well as subcutaneous edema were seen in the area of erythema. Targeted ultrasound of the right axilla showed a lymph node measuring 1.5 cm in diameter with cortical thickening. Ultrasound-guided aspiration of the abscess was performed and 30 mL of purulent fluid was aspirated. The aspirate was sent for cytology and microbiology analysis. Cytology results showed no evidence of malignancy. Culture results showed heavy growth of Actinomyces israelii and Gram positive rods, moderate growth of Gram positive cocci, and numerous WBC.
DIAGNOSIS
Primary actinomycosis of the breast
DISCUSSION
Actinomyces are anaerobic non acid-fast Gram-positive rods. They normally colonize mucous membranes of the mouth, gastrointestinal tract and vagina. Mucosal disruption is the etiology of actinomycosis, be it surgical, traumatic, or via foreign bodies. Actinomyces israelii is the most commonly-found species of the genus and the most common cause of actinomycosis.
Actinomycosis is an indolent, slowly progressive suppurative infection leading to formation of multiple abscesses, dense fibrosis, sinus tracts, and fistulas. Typically, infection is a result of direct extension from colonized mucosa to neighboring tissues. The cervico-facial, thoracic, and abdominopelvic regions are normally involved. Spread is infiltrative due to proteolytic enzyme action. The organism’s size and filamentous structure preclude lymphatic spread; hematogenous spread is likewise rare.1 Actinomyces display a predilection for devitalized tissue.
Actinomycosis occurs very rarely in the breast because of the distance of the breast from the chest wall and natural mucosal habitats of Actinomyces. Primary actinomycosis of the breast refers to inoculation through the nipple, while secondary actinomycosis is a result of extension into the breast from a thoracic infection. Gum disease, poor dentition, and tonsillar infection are notorious sites of origin for actinomycosis.2 Smoking, diabetes, and obesity are risk factors for development of primary breast abscesses.3
Primary actinomycosis of the breast is rare. The clinical presentation includes persistent or recurring infections with abscess formation and breast lump. The presentation may mimic malignancy, including inflammatory carcinoma, and mastitis. Differential diagnosis further includes Staphylococcal mastitis with abscess, tuberculosis, and nocardiosis. Therefore, actinomycosis presents a diagnostic challenge.
Radiologically, actinomycosis may be suspected on the basis of its spread beyond normal tissue and fascial planes. Index of suspicion for actinomycosis is heightened by concomitant lack of or few reactive regional lymph nodes due to ineffective lymphatic spread.
Diagnosis is confirmed by isolation of the organism from a sterile site. The histopathological hallmark of the genus is the formation of branching filaments and sulfur granules composed of a chronic granulomatous response around tangled bacterial elements and tissue debris.4 Identification of Actinomyces species is possible by growing cultures on various types of blood agar.4 Growth is slow with a prolonged latent growth phase, culture should be incubated at least 10 days to rule out positive culture.4
Infections with Actinomyces as sole agent are uncommon as it coexists with other flora in its mucous membrane habitat. Actinomyces can participate in polymicrobial infections involving Bacteroides, Actinobacillus, and Streptococcus.5 The treatment of choice for Actinomycosis is penicillin G or amoxicillin, irrespective of site and severity of infection.6 The infection characteristically improves after a short course of antibiotic treatment but relapses frequently; this is due to the poor penetration of antibiotics into the areas of dense fibrosis associated with the infection.7 Therefore, a prolonged (6-12 month) course of treatment4 as well as frequent monitoring are advised.
This patient possessed a combination of risk factors which predisposed her to both breast abscess and actinomycosis, including morbid obesity and ongoing smoking for the former, and mastitis and biliary tract surgery in the months preceding presentation for the latter. Although she had a history of asthma, she had not been treated with steroids. The infection could have spread from the skin as for the mastitis, but far more likely originated from the gastrointestinal tract in light of her bout of acute cholecystitis. Hematogenous seeding was a likely mechanism of spread of the Actinomyces in this case from the gastrointestinal tract during surgery. The inflammatory vasodilation and edematous congestion in the mastitic breast increased the likelihood of any blood-borne organism to travel to and become lodged in the area of previous breast infection. As such, this appears to be a case of secondary colonization of a previously existing breast abscess with A. israelii.
CONCLUSION
Actinomycosis of the breast is rare. Actinomycosis can masquerade as a malignant process or mastitis clinically and radiologically, and can be readily missed on culture studies. A high index of suspicion must be kept in patients presenting with recurrent breast abscess and the risk factors for actinomycosis, including recent surgery. The utility of isolating Actinomyces from a polymicrobial infection lies in tailoring a treatment plan to this organism, which tends to cause relapsing infection if not pharmacologically eradicated.
REFERENCES
- Brown ML, Drinkwater CJ. Hematogenous infection of total hip arthroplasty with Actinomyces following a noninvasive dental procedure. Orthopedics. 2012 Jul 1;35(7):e1086-9. doi: 10.3928/01477447-20120621-27.
- Porter RS, Kaplan JL (Eds.). The Merck Manual, 19th ed. Merck Sharp & Dohme Corp: New Jersey 2011, 1289-1290.
- Gollapalli V, Liao J, Dudakovic A, Sugg SL, Scott-Conner CE, Weigel RJ. Risk factors for development and recurrence of primary breast abscesses. J Am Coll Surg. 2010; 211:41-48.
- Valour F, Senechal A, Dupieux C, Karsenty J, Lustig S, Breton P, Gleizal A, Boussel L, Laurent F, Braun E, Chidiac C, Ader F, Ferry T. Actinomycosis: etiology, clinical features diagnosis, treatment, and management. Infect Drug Resist. 2014; 5(7):183-197.
- Mandell GL, Bennet JE, Dolin R (Eds.). Principles and practice of infectious diseases, 6th ed., Churchill Livingstone: Philadelphia 2005, 2924-2934.
- Brook I. Actinomycosis: diagnosis and management. South Med J. 2008;101(10):1019-1023.
- Choi MM, Baek JH, Lee JN, Park S, Lee WS. Clinical features of abdominopelvic actinomycosis: report of twenty cases and literature review. Yonsei Med J. 2009;50(4):555-559.
Citation
A S, P G. Primary actinomycosis of the breast. Appl Radiol. 2016;(8):32-34.
August 1, 2016