Diastematomyelia
Images



CASE SUMMARY
A 14-year-old girl presented to the emergency room after mild head trauma. In the emergency room, she was noted to have scoliosis. Nearly 1.5 years after her initial presentation, the patient presented with numbness and tingling in her legs, back pain, weakness of her right leg, and constipation.
IMAGING FINDINGS
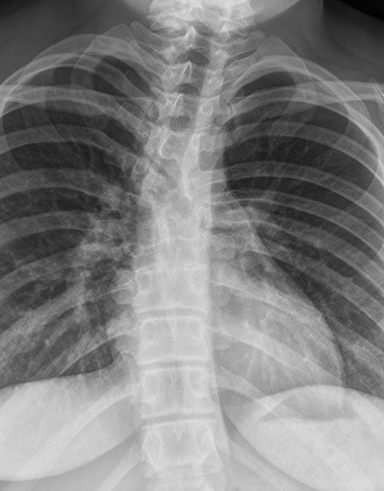
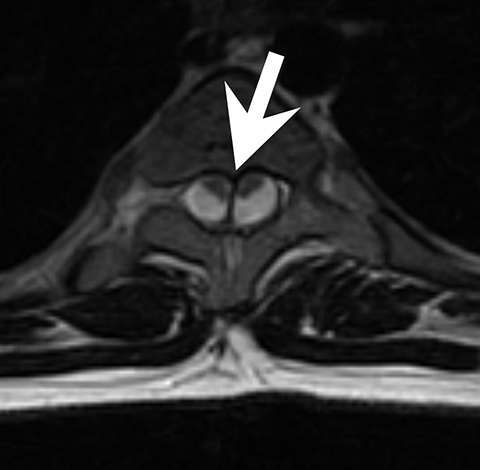
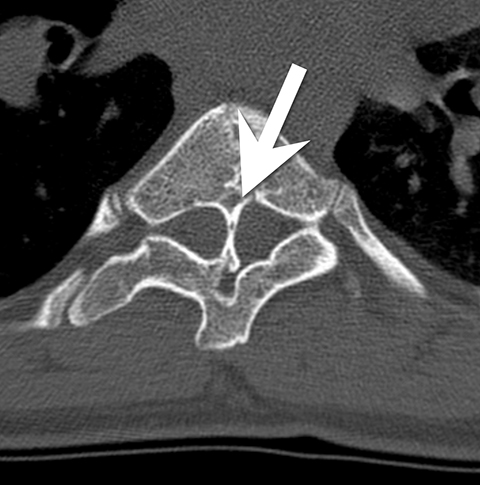
Initially, a scoliosis X-ray was performed. It showed a 15-degree dextroconvex thoracolumbar curvature between the T2 and T12 vertebral bodies. In addition to the curvature, there was a segmentation anomaly involving the T4 through T8 vertebral bodies with possible fusion. An MRI without contrast of the whole spine was then performed. It showed a Chiari 1 malformation, a small syrinx between C7 and T2, and a split spinal cord beginning at the superior aspect of T5 and extending to the superior aspect of T9. A T1-weighted hypointense bony septum was present at midline at the T8 level. Computed tomography showed the same findings, confirming diastematomyelia with a bony septum at T8 and fusion of the T6 through T9 vertebral bodies.
DIAGNOSIS
Diastematomyelia: a type 1 split spinal cord malformation.
The differential diagnosis includes dimyelia (complete spinal cord duplication) and diplomyelia (the presence of an accessory spinal cord).
DISCUSSION
Diastematomyelia is a rare abnormality of the spinal canal characterized by a split spinal cord with or without a bony or fibrous septum. The abnormality most commonly occurs between the T9 and S1 vertebral bodies and is rare within the cervical region.2 Patients may be asymptomatic at birth, but throughout life can develop bowel and bladder dysfunction, motor and sensory difficulties, and progressive pain.3 It is more common in women than men, with some ratios reported as 1.6:1.4
Diastematomyelia occurs as a result of abnormal notochord development and abnormal clefting of the spinal canal that cause the cord to split. Initial classification systems described two distinct types of diastematomyelia. The type 1 deformity is characterized by an extradural bony spur that produces two separate dural sacs with two arachnoid sacs for each separate hemicord. This is the type that usually produces symptoms. Patients are said to have a type 2 diastematomyelia if there is one dural sac surrounding the split cord. While there is no bony spur, these patients can have fibrous septa associated with the split cord. Patients with this type of abnormality are usually asymptomatic.5
Because there was a need to classify diastematomyelia and other conditions with a split spinal cord based on their embryology, a new classification scheme was proposed. Currently these conditions are classified as one of two split spinal cord malformations (SSCM). Type 1 SSCM consists of abnormalities that occur when two hemicords are separated by an extradural bony spur, resulting in two spinal canals and two dural sacs. These abnormalities include most previous definitions of diastematomyelia and occur in fetal development when precursor mesangial cells remain in the accessory neurenteric canal (ANC). The mesangial cells make the medial parts of the hemicords and dural sac while the lateral sac develops. The ANC at that point stays and forms the bony spurs.4 If the ANC would not incorporate mesangial cells, the dural sac is formed by mesenchyme and the ANC regresses, sometimes leaving behind a fibrous spur in the dura.4 Previously, this was termed diplomyelia. Now, diplomyelia is defined as a Type 2 SSCM, anatomically being constituted of one dural sac with two hemicords and one spinal canal. There may be a fibrous band in-between the cords.4
Diastematomyelia has been associated with other neural tube defects, spinal dysraphisms and scoliosis. While patients are often initially asymptomatic, they may present due to visceral malformations, myelomeningoceles, lipomas, Chiari malformations, tethered spinal cords, and other vertebral anomalies. Skin abnormalities such as hypertrichosis are also common.5 Syringomyelia is rarely a concurrent abnormality.2
Spine radiographs may be the first imaging modality to identify an abnormality in patients with diastematomyelia. In these cases, the radiograph may show widening of the spinal canal, a bony ridge at midline, scoliosis and other vertebral anomalies. Currently, CT or MRI is used to confirm the diagnosis. CT scans can show a bony septum and separation of the cord. MRI shows the cord separation and dural sacs in greater detail but may not be as beneficial as CT for the bony abnormalities.1 Prenatal or neonatal ultrasound has been used to identify the split cord as well as the echogenic formation which can indicate a bony spur.3
Asymptomatic patients with diastematomyelia do not require treatment. However, if the patient has symptoms related to the abnormality, they can be treated surgically. Treatment in these patients includes surgery to remove bony spur and reconstruct the dura around the two separated cords.7
CONCLUSION
On presentation this patient did not have any functional defects. Imaging helped to diagnose diastematomyelia, a Type 1 SSCM. The patient’s findings of a Chiari I malformation and scoliosis are associated with her diagnosis of diastematomyelia. Patients are often asymptomatic at birth and do not get motor and sensory dysfunction, along with constipation, until later in life. While this was initially an incidental finding, the use of imaging allowed her to receive proper treatment as soon as symptoms arose.
REFERENCES
- Cheng B., Li F.T., et al. Diastematomyelia: A retrospective review of 138 patients. The Bone and Joint Journal. 2012; 94: 365-372.
- Gan Y.C., Sgouros S., et al. Diastematomyelia in children: Treatment outcome and natural history of associated syringomyelia. Childs Nerv Syst. 2007; 23: 515-519.
- Turgal Mert, Ozyuncu Ozgur, et al. Prenatal diagnosis and clinicopathologic examination of a case with diastematomyelia. Congenital Anomalies. 2013; 53: 163-165.
- Ajayi Olaide, Sadanand Venkatraman, and Asgerzadie Farbod. Type I split cord malformation: Literature review, case presentation and surgical technique. JSM Neurosurg and Spine. 2014; 2: 1026.
- Sonigo-Cohen Pascale, Schmitt Pierre, et al. Prenatal diagnosis of diastematomyelia. Childs Nerv Syst. 2003;19:555-560.
- Saitsu Hirotomo, Yamada Shigehito, et al. Development of posterior neural tube in human embryos. Anat and Embryol. 2004; 209:107-117.
- Martin K., Krastel A., et al. Symptomatology and diagnosis of diastematomyelia of children. Neuroradiology. 1978; 16: 89-90.