Pediatric postoperative intussusception
Images




CASE SUMMARY
A 6-month-old infant presented with increasing abdominal distention over several weeks and was found to have a large heterogeneous mass arising from the left kidney. The patient underwent a left radical nephrectomy, with pathology consistent with congenital mesoblastic nephroma.
Several days following surgical resection, the patient developed diffuse abdominal distention. Dilated small bowel loops on abdominal radiographs were thought to reflect an ileus due to recent surgery. On postoperative day 12, MR angiogram of the renal arteries was performed due to persistent hypertension, and revealed a right lower quadrant ileocolic intussusception, confirmed on subsequent ultrasound examination. Air enema intussusception reduction attempt was unsuccessful, and subsequently, an exploratory laparotomy was performed with successful reduction. The patient recovered well and was discharged home shortly thereafter.
IMAGING FINDINGS
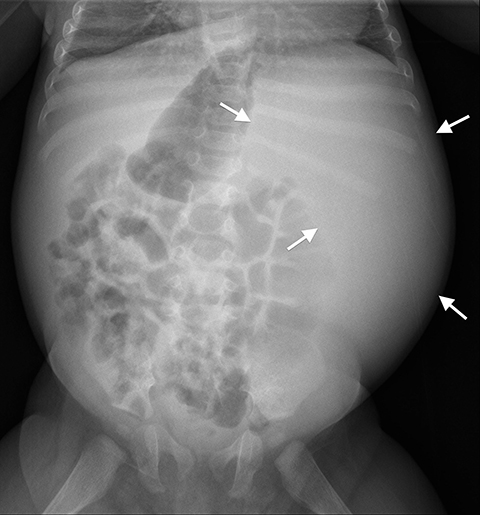
Initial abdominal radiograph on presentation demonstrates a large soft tissue mass in the left abdomen (Figure 1a), corresponding to a large heterogenous mass, which appears to be arising from the left kidney on ultrasound (not shown), confirmed on subsequent MRI of the abdomen (Figure 1B).
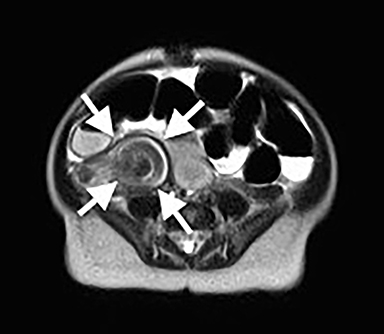
Following left radial nephrectomy, MRI was performed to evaluate for renal artery stenosis, which revealed a right lower quadrant ileocolic intussusception (Figure 2), confirmed on subsequent ultrasound examination (Figure 3).
DIAGNOSIS
Postoperative intussusception
DISCUSSION
Postoperative intussusception (POI) is a rare complication occurring in 0.01 to 0.25% of children following laparotomy,1 accounting for 5-10% of post-operative bowel obstruction.2 It can occur after any type of surgical procedure, even non-abdominal operations, and is most common after extensive bowel manipulation or retroperitoneal dissection. In the majority of cases, no causative factor is identified, although lead points including intestinal tubes, intestinal sutures and inverted appendiceal stumps have been described.3
The pathophysiology of POI remains unclear. Bowel wall edema and altered peristalsis have been implicated, as well as extensive operator manipulation with injury to the serosa, prolonged anesthesia with electrolyte disturbances, and oncologic treatments, such as chemotherapy and radiation.4,5
Although traditionally thought to occur in an older age group than the idiopathic ileocolic intussusception, a more recent systematic literature review of all published cases with clinical information revealed a median age of 19 months.1 This same study showed a male to female ratio of 1.5:1.1 The majority of patients, up to 90%, present within the first two weeks following surgery.3
POI remains a diagnostic challenge to both surgeons and radiologists, and is often overlooked due to its rarity as a complication and nonspecific symptoms, which may mimic a postoperative ileus. Abdominal pain may be masked by pain medication. Vomiting may not be present due to an indwelling nasogastric tube. An abdominal mass may be difficult to palpate due to the laparotomy incision and its associated tenderness. Rectal bleeding rarely occurs. The most common reported symptoms include increased nasogastric output or bilious vomiting and abdominal distention.1
The vast majority of cases are small bowel intussusceptions, accounting for up to 87.2%, with the majority ileoileal, followed by jejunojejunal.1 Ileocolic intussusceptions are present in up to 12.8% of reported cases.1 Cases with multiple sites of intussusception have also been reported in the literature, although uncommon.1 In a single center study, small bowel POI was found to be more common following abdominal surgeries and ileocolic POI more common following non-abdominal surgeries.6
Radiologic diagnosis of POI can be inherently difficult for several reasons. Plain abdominal radiographs are often nonspecific with signs of small bowel obstruction, with ileus as a far more common diagnosis in the setting of recent surgery. As the standard diagnostic examination for idiopathic intussusception, ultrasound can be used to identify POI. However, several factors render the examination more challenging than the typical idiopathic case. Most POIs are small bowel and therefore, can be harder to identify due to small size. Proximally dilated small bowel may cause significant shadowing and limit evaluation of the deeper bowel. Finally, tenderness of a postoperative abdomen can prevent an adequate ultrasound examination. If the ultrasound is negative and a high clinical suspicion remains, a small bowel series can be performed.4 However, this particular examination is often time-consuming, requires coordination, and may be difficult to perform in the post-operative setting. Moreover, a small bowel series may only diagnose the presence of a bowel obstruction rather than demonstrate the intussusception itself. CT can also be used in the diagnosis of POI, although both the small size of the intussusception and relative paucity of mesenteric fat in younger children may render the diagnosis difficult, with poor visualization of the invaginated fat within the layers of the intussusception.4
Due to the proximal small bowel location of most POI, surgical reduction is usually required and rarely involves bowel resection. In cases of ileocolic POI, pneumatic or hydrostatic enema reduction can be attempted, except in those with recent bowel surgery due to the risk of anastomotic disruption. The reported rate of successful enema reduction is generally favorable.1,6
CONCLUSION
Postoperative intussusception (POI) is an uncommon complication in children, which can occur after any type of surgery. POI can be a challenging diagnosis for both surgeons and radiologists, usually presenting with atypical symptoms and most commonly occurring in the small bowel. POI should be considered in cases with prolonged adynamic ileus following surgery. Awareness and early diagnosis are key to reducing the morbidity associated with POI.
REFERENCES
- Yang G, Wang X, Jiang W, Ma J, Zhao J, Liu W. Postoperative intussusceptions in children and infants: a systematic review. Pediatr Surg Int. 2013;29:1273-1279. doi:10.1007/s00383-013-3345-3351.
- Mollitt DL, Ballantine TV, Grosfeld JL. Postoperative intussusception in infancy and childhood: analysis of 119 cases. Surgery. 1979;86:402-408.
- Allbery SM, Swischuk LE, John SD, Angel C. Post-operative intussusception: often an elusive diagnosis. Pediatr Radiol. 1998;28:71.
- Navarro O, Daneman A. Intussusception. Part 3: Diagnosis and management of those with an identifiable or predisposing cause and those that reduce spontaneously. Pediatr Radiol. 2004;34:305-312.
- Kaste SC, Wilimas J, Rao BN. Postoperative small-bowel intussusception in children with cancer. Pediatr Radiol. 1995;1:21-23.
- Klein JD, Turner CG, Kamran SC, Yu AY, Ferrari L, Zurakowski D, Fauza DO. Pediatric postoperative intussusception in the minimally invasive surgery era: A 13-year, single center experience. J Am Coll Surg. 2013;216:1089-1093. doi: 10.1016/j.jamcollsurg.2013.01.059.
Citation
Kim JS, Chun ;J, Kim ;W, Morin ;C, Shet ;N. Pediatric postoperative intussusception. Appl Radiol. 2017;(7):32-33.
July 1, 2017