Muscle beach: Abdominal wall musculature and associated hernias









Hernias of the abdominal wall occur through defects in fibromuscular tissue, which can be congenital or acquired. These areas of weakness lead to defects, which allow intra-abdominal structures to herniate beyond the normal boundaries of the abdominal wall.1 This paper will review common hernias of the abdominal wall, as well as hernias that require more urgent intervention.
Review of hernias
Approximately 80% of all abdominal-wall hernias are inguinal, 5% are femoral, and the other 15% include traumatic, incisional, Spigelian, obturator, lumbar, and paraumbilical types.2 Incisional hernias occur after laparotomy and can occur in 11% to 23% of patients, depending on suturing techniques used.3
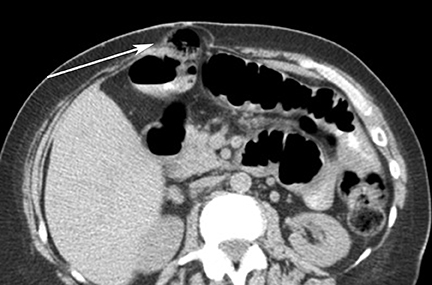
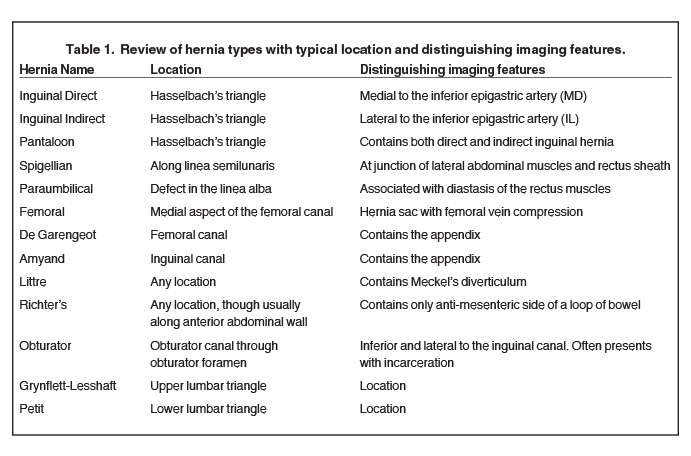
Most abdominal-wall and groin hernias contain fat, with the small bowel being the second most common structure to be found within hernia sacs.1 However, the hernia sac can contain other organs, such as the bladder (Figure 1), gallbladder, or ovaries.1,4 Certain hernias have eponyms. For example, an Amyand’s hernia is an inguinal hernia containing the appendix (Figure 2), a De Garengeot hernia is a femoral hernia containing the appendix, a hernia of Littre contains a Meckel’s diverticulum,5 a Grynflett-Lesshaft hernia occurs through the superior lumbar triangle, while a Petit hernia is a hernia in the inferior lumbar triangle (Table 1).6 A Richter’s hernia is a unique hernia involving only one sidewall of the bowel, usually the anti-mesenteric wall (Figure 3). This type of hernia is associated with high risk of focal bowel ischemia without causing bowel obstruction since contents in the bowel can still pass through the portion of the bowel, which is still within the abdominal cavity.7 Typically, ischemia occurs in the anti-mesenteric side of the bowel since this is the area farthest from the mesenteric blood supply.7
The most common presenting symptom from a groin hernia is a chronic heaviness or a sense of discomfort that is most pronounced during physical activities, such as lifting and running.8 Many patients also notice a focal protrusion, especially when they are standing up or with an increase in intra-abdominal pressure.
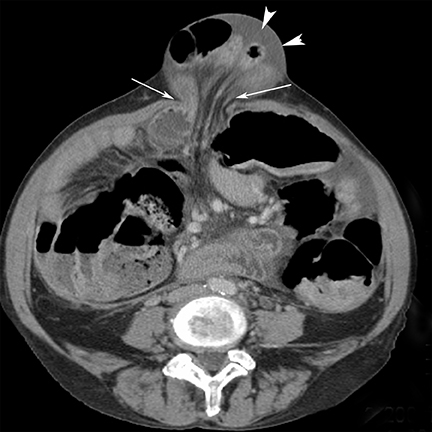
Incarceration or strangulation of tissues can occur with any type of hernia and often requires urgent surgical intervention. This situation occurs more commonly when the hernia defect has a narrow neck. An incarcerated hernia cannot be reduced and may be diagnosed clinically or using sonography (US).9 Incarceration of hernia contents may lead to decreased venous and lymphatic outflow, which results in edema and ultimately may cause ischemia or frank infarction: when this occurs, the term strangulation is used.6 On sonography, color flow documented within the bowel wall can be a helpful sign to differentiate an incarcerated hernia from a strangulated loop.9 The cross-sectional appearance of incarceration is equivalent to a closed-loop obstruction with a “beak sign.”10 Computed tomography (CT) findings suggestive of strangulation include dilated, fluid-filled loops of bowel, located within the hernia sac with hypoenhancement of the wall, surrounding ascites in the hernia sac and mesenteric haziness (Figure 4).6 There is often proximal bowel obstruction as well, unless the patient is vomiting, thus decompressing the proximal small bowel, or in the case of a Richter’s hernia, where only the anti-mesenteric side has become incarcerated in the hernia sac.7
Inguinal hernias
The inguinal canal is a diagonal passage in the lower anterior abdominal wall which measures approximately 4 cm in length and is made up of the aponeuroses of the external oblique, internal oblique, and transversus abdominus muscles.11 A normal inguinal canal contains the ilioinguinal nerve as well as the spermatic cord in men and the round ligament of the uterus in women.11
Inguinal hernias are classified as either direct or indirect. Indirect inguinal hernias are usually congenital and develop at the internal ring.They are hypothesized to arise from defective obliteration of the fetal processus vaginalis.11
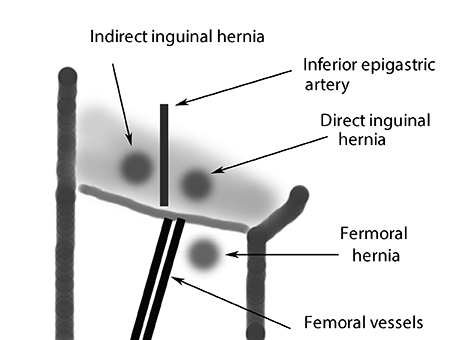
Direct inguinal hernias are usually acquired. They occur through Hasselbach’s triangle, which is anatomically demarcated by the inguinal ligament inferiorly, by the inferior epigastric vessels laterally, and by the rectus abdominus muscle medially (Figure 5).8 A useful sign for differentiating a direct inguinal hernia from a fatty spermatic cord is the “lateral crescent sign” (Figure 6). This occurs when the fat from the direct inguinal hernia compresses the contents of the spermatic cord posteriorly and laterally. On the other hand, in patients with a fatty spermatic cord, the contents of the spermatic cord will be centrally located, surrounded and separated from each other by fat.12
On cross-sectional imaging, the inferior epigastric artery is a useful anatomic landmark for determining whether an inguinal hernia is director indirect. A hernia whose origin occurs medially to the inferior epigastric artery is a direct hernia. An indirect hernia originates laterally to the inferior epigastric artery. A useful mnemonic is “the MD is IL = Medial/Direct, Indirect/Lateral,” using the inferior epigastric artery as the anatomic landmark (Figure 7). A pantaloon hernia is an inguinal hernia with both a direct and indirect hernia occurring on the same side. The spermatic cord is compressed between the two hernia sacs (Figure 6).13
Many causative factors have been suggested for the development of inguinal hernias, including obesity, chronic obstructive airway disease, and benign prostate enlargement. All of these conditions are associated with increased intra-abdominal pressures.14,15 Physical exertion is also a proposed risk factor for inguinal hernia formation.16,17 In the prospective study by Smith GD et al, which evaluated inguinal hernias,7% of their cohort attributed their hernia to a single strenuous event.18
Femoral hernias
While inguinal hernias are more common in men, with a ratio of 9:1, femoral hernias occur more commonly in women, with a ratio of 4:1.19 Femoral hernias develop in the empty space at the medial aspect of the femoral canal and are more commonly seen in women. Pectineus muscle atrophy may contribute to femoral hernia development, creating a potential space for the hernia to form.19 Up to 40% of femoral hernias present with obstruction or incarceration (Figure 8).19
The combination of a localized hernia sac with femoral vein compression is a useful distinguishing feature of femoral hernias compared to inguinal hernias. A study by Suzuki et al reported the imaging finding of femoral vein compression in 100% (7/7) of femoral hernias compared to 45% in inguinal hernias.20
Cross-sectional imaging of hernias
Sonography is often the first imaging modality used to evaluate patients with suspected groin or ventral hernia. The sensitivity and specificity of detecting groin hernias with sonography is > 90%.21,22 In another study by Lilly et al, the authors were able to correctly identify inguinal hernias as direct or indirect with 85% success compared to surgical findings.23
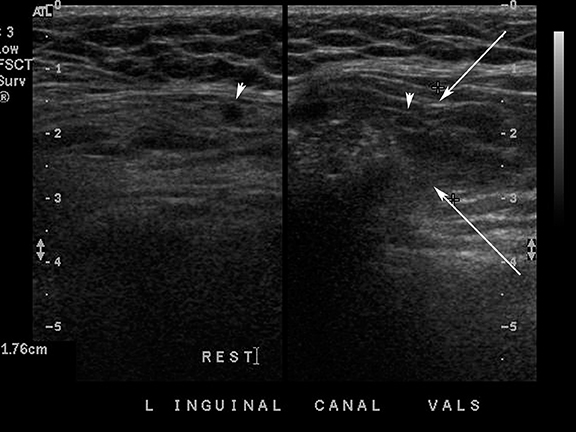
Advantages of sonography include availability, portability, low cost, and lack of exposure to ionizing radiation. The capability of real-time imaging is of paramount importance as patients can direct the attention of the radiologist and sonographer to the region of concern and perform maneuvers to increase visibility of the hernia. Sonographic evaluation usually starts with a low-frequency curved probe (3.5 MHz-5MHz), which is particularly important in overweight patients since the hernia may be beyond the depth of penetration of the high frequency transducers. A secondary focused exam is performed with a high-frequency linear probe (7.5 MHz-10 MHz). Supine imaging using Valsalva maneuvers as well as upright scanning often help to identify intermittent or sliding types of hernias (Figure 9). If small bowel loops are present in the hernia sac, these can usually be identified with sonography as they have the typical multi-layered gut signature (Figure 10).Cine clips can be obtained for comparison to the unaffected side.
Sonographic evaluation after hernia repair can be challenging due to dense shadowing caused by the surgical mesh; however, superficial seromas and hematomas can be identified post-operatively in up to 20% of cases.24 Most cases of recurrent hernia occur along the edge of the repair and can be identified during scanning using Valsalva maneuvers. In cases of suspected complications, such as intra-abdominal abscess, bowel obstruction, or ischemic bowel, CT should be considered the imaging modality of choice.6
Advantages of CT include its high spatial and contrast resolution and multi-planar capability, which allows accurate characterization of hernia types and can provide alternate diagnoses, such as hematoma, abscess or tumor when patients present with non-specific symptoms.Three-millimeter multi-planar reconstructions are preferred for interpretation purposes. Either positive or negative oral contrast may be used to better visualize bowel loops. If there is clinical suspicion for bowel ischemia, positive oral should not be used since the dense oral contrast may impede visualization of reduced bowel wall enhancement. In cases of suspected vascular compromise (strangulated hernia), use of intravenous contrast material is necessary.6
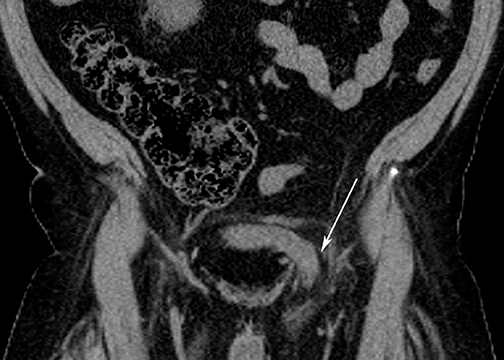
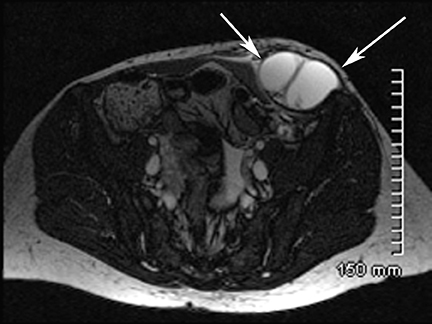
Magnetic resonance imaging (MRI) can detect and characterize hernias, as well as differentiate inguinal from femoral hernias with a high sensitivity and specificity (Figure 11).21 Potentially useful sequences include coronal 3-dimensional T1W VIBE (Volume Interpolated Breath Hold, Siemens) without fat saturation during Valsalva and at rest, as well as axial TSE T2 and Axial STIR (short Tau inversion recovery), including both groins for comparison. Advantages include lack of ionizing radiation and characterization of hernias without IV contrast. Disadvantages include cost, increased imaging time, and the inability to image in real-time. Therefore, in many centers, assessment of hernias with MRI remains limited to special cases.
Other abdominal-wall hernias
Obturator hernias are rare but generally occur in thin, elderly women. Due to their location deep in the lateral pelvis, CT is the imaging modality of choice to evaluate this type of hernia. The sina que non on CT is visualization of the bowel entering obturator canal through the obturator foramen, which is inferior and lateral to the inguinal canal. Obturator hernias often present with symptoms of acute bowel obstruction due to incarceration. (Figure 12).25
Spigelian hernias occur along the linea semilunaris, which is a continuation of the aponeuroses of the layered lateral abdominal muscles and the rectus abdominis sheath (Figure 12). The semilunar line extends from the cartilage of the ninth rib to the pubic spine and is an area of congenital weakness.26 Despite the location of Spigelian hernias in relation to the abdominal musculature, this type of hernia is not generally related to physical activity and can be distinguished on CT from other types of hernias by its anatomic location (Figure 13).7
Paraumbilical hernias often arise from large defects of the linea alba in the region of the umbilicus and are often related to diastasis of the rectus abdominus muscles (Figure 4).6
Traumatic hernias are rare, but have been associated with high-impact blunt trauma (eg high-velocity motor vehicle accidents or sports injuries, such as downhill skiing or mountain biking) that produces increased intra-abdominal pressure sufficient to disrupt the abdominal wall musculature.27
Conclusions
Inguinal hernias are the most common type of hernias in the North American population. Paraumbilical and inguinal hernias may develop as a result of a sudden strain or with athletic activities but often arise without any identifiable causative event.
Femoral hernias and obturator hernias are more commonly associated with complications such as bowel obstruction and strangulation,due to their anatomic location. Richter’s hernias are uncommon, but the focal herniation of the anti-mesenteric side of the bowel predisposes patients to ischemic bowel changes without associated obstruction.
Sonography is the preferred modality used for assessment of inguinal hernias due to lack of ionizing radiation and directed scanning over the area of pain. Use of positional or Valsalva maneuvers with a high-frequency probe yields > 90% accuracy in identifying hernias in the groin region. In locations other than the groin or in cases with concerning clinical features, such as obstruction or ischemia, CT is preferred as the initial imaging modality.
REFERENCES
- Pans A. New prospects in the etiology of groin hernias. Chiurgie. 1999;124:288-297.
- Richards AT, Quinn TH, Fitzgibbons RJ Jr. Abdominal wall hernias. In: Greenfield LJ, ed. Surgery. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2001:1185-1223.
- Cassar K, Munro A. Surgical treatment of incisional hernia. Br J Surg. 2002;89:534-545.
- Gurer A, Ozdogan M, Ozlem N, et al. Uncommon content in groin hernia sac. Hernia. 2006;10:152-155.
- Hutchinson B. Amyand’s hernia. J R Soc Med. 1993;86:104-105.
- Aguirre DA, Santosa AC, Casola G, Sirlin CB. Abdominal wall hernias: Imaging features, complications, and diagnostic pitfalls at multi–detector row CT. Radiographics. 2005;25:1501-1520.
- Skandalakis PN, Zoras O, Skandalakis JE, Mirilas P. Richter hernia: Surgical anatomy and technique of repair. Am Surg. 2006;72:180-184.
- Brooks DC, Turnage R, Pories SE. Classification and diagnosis of inguinal and femoral hernias. Updated 2010 literature review version. 2010;18.2.
- Kulstad E, Pittman L, Konicki P.J. Ultrasound in the diagnosis of incarcerated hernia. The Internet Journal of Emergency Medicine. 2003;1. DOI: 10.5580/2229.
- Balthazar EJ, Birnbaum BA, Megibow AJ, et al. Closed-loop and strangulating intestinal obstruction: CT signs. Radiology. 1992;185:769-775.
- Bhosale PR, Patnana M, Viswanathan C, Szklaruk J. The inguinal canal: Anatomy and imaging features of common and uncommon masses. Radiographics. 2008;28:819-835.
- Burkhardt JH, Arshanskiy Y, Munson JL, Scholz FJ. Diagnosis of inguinal region hernias with axial CT: The lateral crescent sign and other key findings. Radiographics. 2011;31:E1-E12.
- Steadman’s Medical Dictionary. 28th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2005.
- Read RC. Metabolic factors contributing to herniation: A review. Hernia.1998;2:51-55.
- Sorensen LT, Friis E, Jorgensen, et al. Smoking is a risk factor for recurrence of groin hernia. World J Surg. 2002;26:397-400.
- Carbonell JF, Sanchez JL, Peris RT. Risk factors associated with inguinal hernias: A case control study. Eur J Surg. 1993;159:481-486.
- Kang SK, Burnett CA, Freund E, Sestito J. Hernia: Is it a work-related condition? Am J Ind Med. 1999;36:638-644.
- Smith GD, Crosby DL, Lewis PA. Inguinal hernia and a single strenuous event. Ann R Coll Surg Engl. 1996;78:367-368.
- McIntosh A, Hutchinson A, Roberts A, Withers H. Evidence-based management of groin hernia in primary care--a systematic review. Fam Pract. 2000;17:442-447.
- Suzuki S, Furui S, Okinaga K, et al. Differentiation of femoral versus inguinal hernia: CT findings. AJR Am J Roentgenol. 2007;189:345.
- Van den Berg JC, de Valois JC, Go PM, Rosenbusch G. Detection of groin hernia with physical examination, ultrasound, and MRI compared with laparoscopic findings. Invest Radiol. 1999;34:739-743.
- Korenkov M, Paul A, Troidl H. Color duplex sonography: diagnostic tool in the differentiation of inguinal hernias. J Ultrasound Med. 1999;18:565-568.
- Lilly MD, Arregui ME. Ultrasound of the inguinal floor for evaluation of hernias. Surg Endosc. 2002;16:659-662.
- Parra JA, Revuelta S, Gallego T, et al. Prosthetic mesh used for inguinal and ventral hernia repair: Normal appearance and complications in ultrasound and CT. Br J Radiol. 2004;77:261-265.
- Haraguchi M, Matsuo S, Kanetaka K, et al. Obturator hernia in an ageing society. Ann Acad Med Singapore. 2007;36:413-415.
- Martin M, Paquette B, Badet N, et al. Spigelian hernia: CT findings and clinical relevance. Abdom Imaging. 2012. [Epub ahead of print].
- Netto F, Spencer AC, Hamilton P, et al. Traumatic abdominal wall hernia: Epidemiology and clinical implications. J Trauma. 2006;61:1058-1061.
