Left mesial temporal sclerosis (MTS)


Prepared by Rebecca Spiegel, MD, MA and Edward Y. Lee, MD, MPH from the Department of Neurology, Albert Einstein College of Medicine, Bronx, NY.
Case summary
A 6-year-old boy with a 5-year history of intractable complex partial seizure was referred by his neurologist for a presurgical evaluation of a brain locus that may have triggered the seizures. The seizures were described as starting with vocalizations that would quickly convert to convulsions of all four extremities. Afterward, the patient would become aphasic or dysarthric for approximately 1 minute; then the patient would become sleepy.
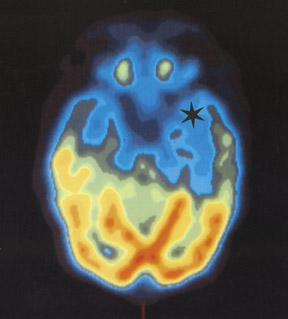
The patient had been on multiple seizure medications in the past. All of the seizure medications had proven to be ineffective in completely controlling his seizures. On average, the seizure frequency was 5 to 8 times per month. His physical examination was significant for fairly marked hyperactivity and compulsive behavior, such as repeated counting. He was also found to have mildly reduced language fiuency as compared with that expected for his age. The rest of his examination was unremarkable. The patient's presurgical work-up included an electroencephalography (EEG), which revealed intermittent left temporal slowing, suggestive of either a postictal state or a structural abnormality in this region. In addition, the patient underwent magnetic resonance imaging (MRI) (Figure 1) and positron emission tomography (PET) (Figures 2 and 3).
Imaging Findings
MRI of the brain shows brain parenchymal volume loss of the left hippocampus, which is compatible with mesial temporal sclerosis (Figure 1). Axial and coronal brain PET shows decreased F-18 fiuorodeoxyglucose (FDG) uptake in the left temporal lobe, which is consistent with the MRI finding of left-sided mesial temporal sclerosis (Figures 2 and 3).
Diagnosis
Left mesial temporal sclerosis (MTS)
Discussion
While MTS is the most common symptomatic pathologic entity in adult and adolescent patients with seizures of temporal lobe origin, it is considered to be a rare pathologic finding among infants and young children. 1-3 The etiology of MTS is still not fully understood. However, there is now considerable evidence, from both animal and clinical studies, that has shown that MTS is not only the cause of seizures, but is also the result of seizures. 4 Animal studies suggest that the mechanism by which seizures can cause MTS is through the release of excitatory amino acids, primarily glutamate. 4 These excitatory amino acids lead to prolonged neuronal depolarization and result in the entry of cytotoxic amounts of calcium, which can eventually lead to sclerosis. Clinical studies also suggest that prolonged seizures are a risk factor for MTS and that a period of time is required for the lesions to fully develop. 4
Clinical presentation of MTS in adults and adolescents is characterized by auras that often involve visceral sensation, motionless stare, loss of awareness, and oral alimentary automatism. 5 Infants typically do not have any identifiable auras, present with seizures that are of longer duration (>1 minute), and have more prominent convulsive activity. Moreover, infants predominately present with behavioral arrest with possible impairment of consciousness. Their automatism is mostly discrete and predominantly orofacial. 3
MRI is the radiological investigation of choice for the evaluation of patients with MTS, since it can identify structural abnormalities. 6 However, other MR techniques, such as magnetic resonance spectroscopy (MRS) and functional MRI (fMRI) are also being increasingly used in the diagnosis of MTS. MR spectroscopy can detect metabolic abnormalities, while fMRI allows for the noninvasive evaluation and localization of cognitive, motor, and sensory deficits that are associated with MTS. Also, intraoperative MRI-based image-guided systems are now used as an adjunct in the surgical treatment of MTS for better anatomic localization. 7
Along with MRI, the use of PET scans with FDG is also well-established for the diagnosis of MTS. In the interictal state, the epileptogenic temporal lobe indicates decreased glucose metabolism in approximately 80% of these patients. Moreover, PET scans may be a reliable indicator of clinical outcome postsurgery; the presence of a hypometabolic temporal lobe is a favorable prognostic indicator. 8
Antiepileptic drug treatment for patients with MTS is effective in the suppression of secondarily generalized seizures. However, 50% of patients continue to have partial attacks. With combined use of MRI, PET, and video-EEG, we can properly select patients who can benefit from anterior temporal lobe resection. In such patients, complete seizure control is achieved in >80% of cases. 4 Patients who had an earlier age of onset and a low number of previously used antiepileptic agents have an overall better outcome after surgery. 9
Conclusion
Mesial temporal lobe sclerosis contributes to a significantly compromised quality of life of many patients. Antiepileptic agents offer complete seizure control in only a minority of these patients. However, with the aid of MRI and PET scans, patients can now be selected to undergo anterior temporal lobe resection, a procedure that leads to seizure control in a majority of patients.
