Imaging sports-related elbow injuries
Images








With increasing participation in organized sports, the incidence of sports-related injuries is on the rise in males and females of all ages. The elbow is one of the more commonly injured joints, especially in sports associated with throwing, swinging, or punching motions. Many sports-related injuries of the elbow are secondary to chronic overuse, which typically results from microscopic damage of tissues secondary to chronic submaximal loading.1,2 Elbow injuries are also common in myriad sports where participants experience blunt trauma or falls onto an outstretched hand. Knowledge of the patient’s age is important to understanding the prevalent injuries in adults, adolescents and children. Pediatric patients are more prone to a specific subset of injuries, given their unique anatomy and intensity of training in sports such as baseball and gymnastics.2-4 Adults also have a high incidence of elbow injuries related to sports, although the etiologies and mechanisms are slightly different.
Imaging modalities
Radiography remains the best initial imaging approach for evaluating elbow pain: anteroposterior (AP), lateral, and internal and external rotation views are considered standard.5 Radiographs are effective in demonstrating fractures, dislocations, joint effusion/hemarthrosis and soft tissue swelling. Although radiographs are essential in the initial workup of musculoskeletal injury, cross-sectional imaging may occasionally be sought to further define the extent of injury.1,5
Sonography is a relatively inexpensive, portable and widely available means to evaluate the elbow. Sonography is useful in evaluating the elbow in athletes, particularly when it comes to assessing ligamentous and tendinous injuries, and identifying effusions.6 Sonography is gaining more widespread acceptance as a primary musculoskeletal imaging modality, is best performed by experienced operators, and is helpful in guiding percutaneous therapeutic injections.7
Computed tomography (CT) may be indicated in evaluating complex osseous injury after initial radiographs. CT arthrography after intraarticular injection of iodinated contrast is an alternative to MRI and sonography in assessing tendons and ligaments.8 Images are obtained in the axial plane with 2D sagittal and coronal and 3D surface rendered reconstructions available for surgical planning. Disadvantages of CT include ionizing radiation to the patient as well as suboptimal characterization of soft tissue pathology compared to MRI.
Magnetic resonance imaging (MRI) has emerged as the imaging modality of choice for evaluation of elbow pain in athletes.8 MR imaging provides excellent spatial resolution and soft tissue contrast, and can detect subtle pathology in the soft tissues and bone marrow. Images are typically obtained in axial, coronal oblique and sagittal oblique planes relative to the transepicondylar axis. Standard sequences include T1-weighted, proton density (PD) and T2-weighted images with fat suppression (FS). 2D or 3D gradient echo sequences can be used to better visualize the cartilage, and allow an infinite number of reconstructions when volumetrically acquired.8 Imaging field-of-view should be about 12 cm and extend from the distal humerus to the bicipital tuberosity of the radius, and a dedicated elbow coil should be used for optimal spatial resolution.9 Patients can be positioned in the MR scanner in either the “superman position” (arm above head with elbow in the center of the bore), or supine with the elbow positioned at the side. The superman position provides superior field homogeneity, but can only be utilized if the patient can tolerate this position without moving.10 MR arthrography is selectively performed for increased accuracy in detecting ulnar collateral ligament tears, osteochondral defects and intraarticular bodies.11,12 MRI disadvantages include increased scan times and relatively high cost compared to other imaging modalities.
Soft-tissue injuries
Tennis elbow
Tendon pathology involving the common extensor tendon origin is the most common cause of elbow pain and/or disability, and is much more common than tendinous injury of the common flexor tendon origin. “Tennis elbow,” “lateral epicondylosis” and “lateral epicondylitis” are synonymous terms for this degenerative process caused by repetitive microtrauma; however, most afflicted patients do not play tennis, and epicondylitis is a misnomer since this entity is not caused by inflammatory change.13 Tennis elbow is usually seen in the 4th or 5th decade of life with equal prevalence among men and women.13,14 Although classically associated with racket sports like tennis, most patients with this disease have never played tennis. Patients present clinically with pain and point tenderness overlying the lateral epicondyle and pain with resisted wrist extension (Cozen’s sign).14
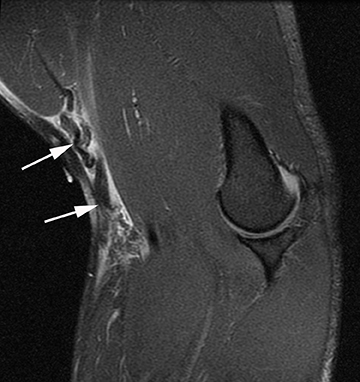
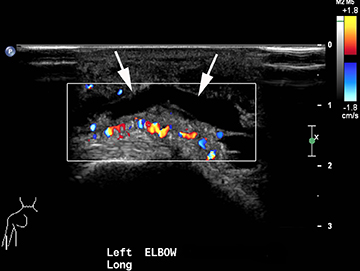
Tennis elbow is a clinical diagnosis and typically does not necessitate imaging. Findings include thinning, partial tearing or avulsion of the common extensor tendon origin at the lateral epicondyle.13 Partial tears of the lateral ulnar collateral ligament may also be found in conjunction with common extensor tendon tears in more advanced cases.13,14 Sonography or MR imaging may be obtained in cases of refractory elbow pain in patients who fail conservative treatment measures, in order to exclude other causes of chronic elbow pain such as lateral collateral ligamentous injury. The common extensor tendon is optimally imaged with sonography with the elbow flexed and forearm pronated. Transverse and longitudinal images should be obtained from the tendinous insertion to the extensor carpi radialis (ECRB) myotendinous junction. Thickening and heterogeneity are signs of tendinosis, whereas with a partial- or full-thickness tear there will be evidence as anechoic, fluid-filled tendinous gaps. Varying degrees of hyperemia can be seen with Doppler imaging, representing inflammation associated with the reparative process.14,15 Furthermore, ultrasound-guided therapies for tennis elbow and other tendinopathies have become more widespread. Percutaneous treatments include dry needling, as well as injection of steroids, platelet-rich plasma (PRP), autologous conditioned plasma and whole blood.16,17 Tendinosis of the common extensor tendon will be evident on MRI as thickening and intermediate T1- and T2-weighted signal intensity, whereas partial- or full-thickness tears will demonstrate fluid signal within the discontinuous portion of the tendon (Figure 1).18,19
Injuries to the radial collateral ligament (RCL) complex can occur in conjunction with advanced cases of tennis elbow as well as sports-related trauma leading to posterolateral rotary subluxation of the elbow.20-23 The radial collateral ligament complex is comprised of the radial collateral ligament proper, the lateral ulnar collateral ligament and annular ligament. Of these, the LUCL is the most important in stabilization and dynamic sonographic evaluation and MRI can be useful in its evaluation.20,21-23 Tears of the lateral ulnar collateral ligament usually occur at the humeral origin, and will be evident as discontinuous fibers with surrounding edema or hemorrhage. Of note, failure to recognize lateral ulnar collateral ligament (LUCL) tears prior to surgical treatment of tennis elbow will lead to persistent postoperative symptoms.
Golfer’s elbow
Common flexor-pronator tendon origin pathology in middle-aged and older individuals is also referred to as golfer’s elbow. This entity is characterized by repetitive overuse and microtearing of the flexor-pronator tendons, with progressive degeneration due to an immature reparative response.18 This disease typically occurs in the fourth and fifth decades of life, is 7-10 times less common than tennis elbow, and commonly affects golfers, bowlers, swimmers, tennis players, and throwing athletes.18 Clinically, patients present with insidious medial elbow pain and weakness in grip strength.19,24
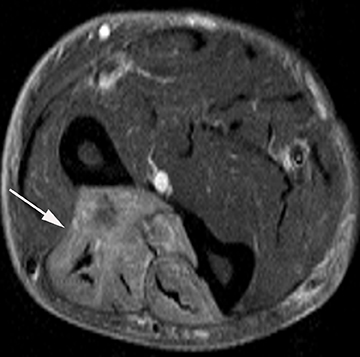
Sonography and MRI can confirm the diagnosis in patients with refractory medial elbow pain and exclude other etiologies. Sonography demonstrates an enlarged and hypoechoic common flexor tendon origin in the presence of tendinosis, whereas MR imaging depicts thickening and intermediate signal intensity of the common flexor-pronator muscle group (Figure 2).25 The ulnar collateral ligament should also be carefully evaluated, since UCL tears may be associated with refractory cases of golfer’s elbow due to persistent instability. Finally, chronic focal stress at the common flexor tendon origin can lead to medial traction enthesophytes.24,25
Pitcher’s elbow
Forces upon the elbow are most marked during the acceleration phase of throwing, and can result in medial tension overload, lateral compression and extension overload. Medial elbow pain caused by excessive valgus forces and high pitching velocities can occur in overhead throwing athletes of all ages. Usually due to excessive pitch counts or poor technique, up to 20% of baseball pitchers between the ages of 9 and 15 will experience elbow pain at some point.4 Injury to the ulnar collateral ligament, also known as the medial collateral ligament, is a common cause of medial elbow pain and valgus instability in athletes. The UCL is made of anterior, transverse and posterior bundles, and is most often injured following acute or recurrent valgus stress of the elbow.26,27 Injuries have been documented in baseball and American football players (especially pitchers and quarterbacks), track and field athletes (particularly javelin throwers), and those who play volleyball, golf and polo.28
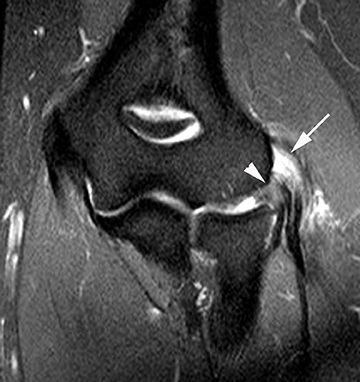
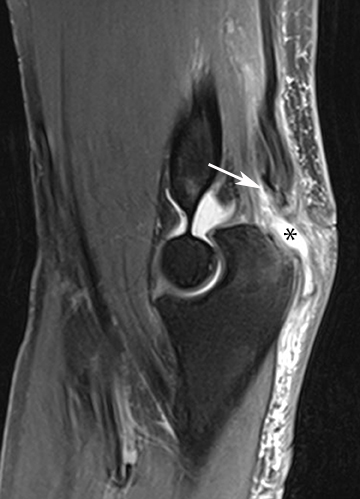
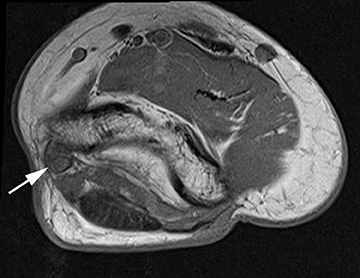
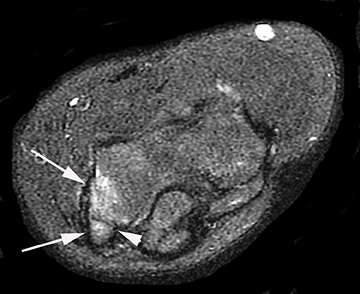
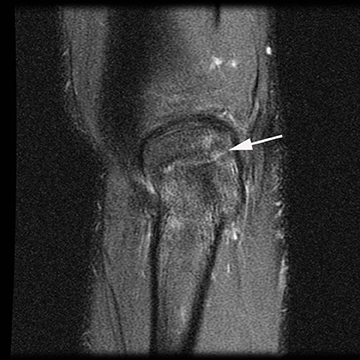
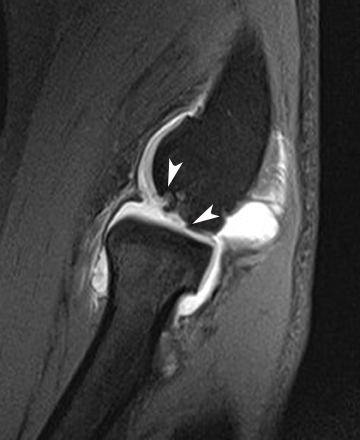
There are several modalities which can be used to image the ulnar collateral ligament including radiography, sonography, CT arthrography and MRI. Stress radiography can demonstrate widening of the ulnohumeral joint, and heterotopic ossification of the UCL can be seen with chronic injuries. Sonography may demonstrate hypoechoic and thickened ligaments with tendinosis, as well as classic findings for partial or complete ligamentous disruption. MRI may demonstrate increased T2-weighted signal within the ligament (commonly within the anterior band) or hyperintensity within the sublime tubercle (Figure 3). Insinuation of arthrographic contrast into articular sided tears may occur anywhere along the tendon and may result in a “T sign” when contrast extends in the interval between the sublime tubercle and stripped ligamentous attachment; complete rupture will show extravasation of contrast through the ligamentous defect.25,28
Preoperative MR imaging has been shown to predict rehabilitation outcomes of UCL injuries in baseball players, and postoperative MRI is helpful when difficulties arise.29 Reconstruction of the UCL has been famously named “Tommy John” surgery, and complications from surgery include avulsion fractures of the medial epicondyle, graft degeneration and tearing.30,31 Avulsion fractures and stress reaction of the medial epicondyle at the origin of the UCL and the sublime tubercle at the insertion of the UCL have also been described in throwing athletes and gymnasts, and will be discussed later.32, 33
Biceps tendon pathology
The biceps brachii tendon is vital for flexion and supination of the upper extremity, and spans both the shoulder and elbow joints.34 For this reason, biceps tendon pathology is usually separated into proximal (ie, shoulder) and distal (ie, elbow) components. Biceps tendon injuries are associated with sports, especially those that involve throwing, forced elbow flexion or overhead activities. Injuries of the distal biceps are much less common than those of the proximal biceps, accounting for approximately 3% of the biceps tendon injuries.35,36 Football players, weightlifters and bodybuilders have the highest prevalence of distal biceps tendon injuries, and risk further increases in men, smokers and those using anabolic steroids.34-38
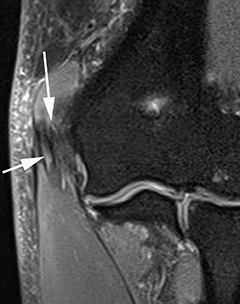
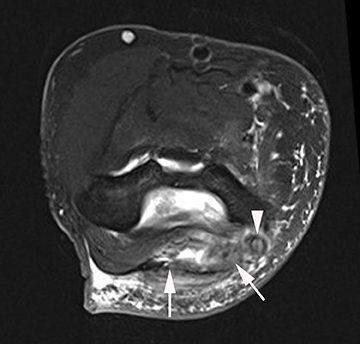
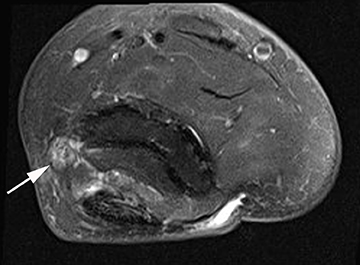
It is important to diagnose biceps tendon tear early, as a surgical delay can lead to chronic weakness. Evaluation of the biceps tendon can be accomplished with sonography or MRI. Sonographically, the distal biceps tendon is imaged by placing the ultrasound probe in the antecubital fossa with the elbow extended and the forearm supinated (36. Injuries of the distal biceps tendon usually occur near the insertion onto the radial tuberosity, are more commonly partial thickness and can involve either the long or short head.39 MR imaging is useful in presurgical planning of full-thickness tears, and the radiologist should report the degree of proximal retraction and the quality of the tendinous remnant (Figure 4).38-40 Of note, the tendon rarely retracts significantly into the arm because it is partially tethered by the bicipital aponeurosis, also known as the lacertus fibrosis.
Triceps tendon pathology
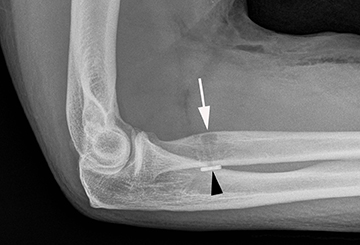
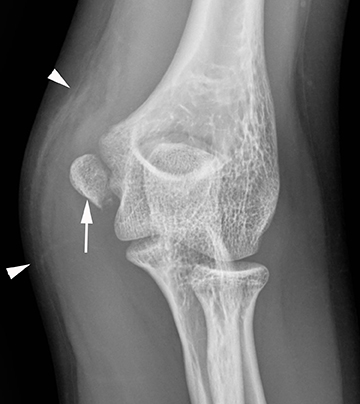
Injuries of the triceps tendon are exceptionally rare, with a reported prevalence of between 1% and 3.8%.41 Triceps tendon tears usually occur near the insertion onto the olecranon and are often related to an acute traumatic event. Injuries have been reported with weightlifting, American football, soccer and rugby. Patients often present clinically with swelling of the posterior elbow following a fall on an outstretched hand.41-43 On radiography, triceps tendon rupture will present with soft tissue swelling overlying the olecranon and, occasionally, a small olecranon avulsion fragment (Figure 5). Sonography can assess the integrity of the triceps tendon, avulsion fractures and any associated fluid collections or olecranon bursitis. Morphologic and signal intensity changes of the triceps tendon are similar to those of other tendons as previously described.38,45 Triceps tendon rupture can be partial or complete, can range from millimeters to centimeters in width, and almost always involve the lateral head insertion. MRI may provide added value due to the association of radial head fracture, capitellar fracture and ulnar collateral ligament rupture with triceps injuries (Figure 5).44,45
Olecranon bursitis
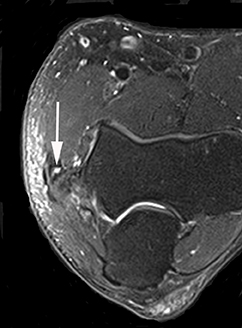
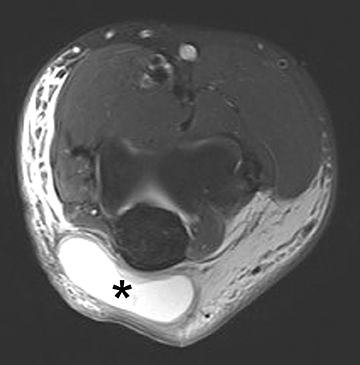
The olecranon bursa is a fluid filled sac-like structure that acts as a cushion, allowing the posterior skin of the elbow to glide past the olecranon process with minimal friction.46,47 Inflammation of the olecranon bursa commonly occurs in athletes who participate in sports that require repetitive elbow extension and flexion such as baseball, swimming and weight lifting.46 Direct trauma to the posterior elbow from falling on a hard surface such as hardwood, ice, or turf can also cause the olecranon bursa to become inflamed.46 The clinical presentations of olecranon bursitis can range from a minor painless fluctuant mass to a painful erythematous swelling that limits elbow mobility.46 Lateral radiographs may delineate the extent of soft tissue swelling overlying the olecranon process.47 Sonography may reveal a hypoechoic, fluid-filled bursa, and MRI will demonstrate hypointense T1- weighted fluid with variable signal intensity on T2-weighted sequences (Figure 6).46-48
Cubital tunnel syndrome
Nerve entrapment and compression syndromes of the elbow include cubital tunnel syndrome, radial tunnel syndrome, posterior interosseous nerve syndrome, anterior interosseous nerve syndrome and pronator syndrome.49 Cubital tunnel syndrome is the most common entrapment neuropathy of the elbow, and has several etiologies including throwing sports, tennis, and volleyball.28 Traction injuries to the ulnar nerve can occur secondary to the dynamic valgus forces of throwing. Compression of the ulnar nerve within the cubital tunnel can occur secondary to direct trauma, repetitive stresses or replacement of the overlying retinaculum with an anomalous anconeus epitrochlearis muscle, which is found in 11% of the population.5,10,50 Recurrent subluxation of the nerve due to acquired laxity from repetitive stress or trauma can lead to friction neuritis. Finally, osseous spurring within the ulnar groove caused by overuse and posteromedial impingement in throwers can cause nerve irritation.51 Ulnar nerve thickening and increased T2-weighted signal are typical MRI features of cubital tunnel syndrome (Figure 7). Edema-like signal changes or atrophy of the flexor carpi ulnaris and flexor digitorum profundus muscles may also be secondary to ulnar neuropathy.49
Radial nerve entrapment
Radial nerve entrapment at the elbow can be subdivided into two major categories: radial tunnel syndrome and posterior interosseous nerve syndrome (PINS).49 The posterior interosseous nerve is a deep branch of the radial nerve in the forearm that can be compressed from repetitive gripping combined with supination in weight lifters and swimmers. The superficial head of the supinator muscle along the arcade of Frohse is the most common site of nerve entrapment, where a thick fibrous band may exist along the arcade of Frohse.49 It is important to note that a small percentage of radial neuropathy cases have associated lateral elbow symptoms related to common extensor tendon pathology.49 MR imaging manifestations of PINS includes thickening and increased T2 signal of the nerve fibers, as well as edema-like signal changes in the innervated extensor compartment musculature in the acute and subacute setting, and atrophy in the chronic stages (Figure 8).
Osseous trauma
Medial epicondyle apophysitis and avulsion injuries
Medial elbow pain is a common complaint in Little League baseball players between the ages of 9 and 12 years, and is often secondary to stresses placed upon the epicondylar apophysis. In skeletally immature patients, the UCL is much stronger than the apophyseal growth plate. Therefore, varying degrees of fragmentation and separation of the medial epicondyle at the apophysis can occur in the setting of chronic valgus stress (Figure 9). Clinical findings include medial elbow pain after throwing without valgus instability.52 Medial epicondylar apophyseal hypertrophy with fragmentation and apophyseal separation can be seen in symptomatic patients on radiographs and sonography, although one study has demonstrated this finding in asymptomatic patients as well.53 MR imaging may demonstrate increased T2-weighted signal in the medial apophysis and within or around the common flexor tendon (Figure 9).54
Sublime tubercle stress fracture
Avulsion fractures of the sublime tubercle of the ulna have been reported in throwing athletes with chronic medial elbow pain, although these are much less common than injuries to the ulnar collateral ligament complex.32,33 Sublime tubercle fractures and stress responses occur near the attachment of the ulnar collateral ligament and are caused by repetitive valgus elbow force. MRI will show an intact ulnar collateral ligament, with the point of failure being the osseous fracture (Figure 10).
Olecranon stress fractures
Olecranon stress fractures caused by chronic impingement and shear forces in the posterior compartment are most commonly encountered in throwing athletes. Repetitive valgus stress on the elbow in the late stages of throwing combined with rapid elbow extension result in olecranon micro-trauma. Repetitive excessive forces may eventually lead to olecranon stress fractures propagating from the structural weak point in the trochlear groove, and may be detected on radiographs as transverse or oblique in orientation, with or without sclerotic changes.55 MR imaging is reserved for cases where radiographs are inconclusive, and will unequivocally establish the diagnosis by demonstrating the fracture line and associated bone marrow edema (Figure 11). Initial treatment of olecranon stress fractures consists of rest and temporary splinting. Surgical management with screw fixation may be preferable in order to achieve early union in elite athletes and avoid prolonged immobilization.56,57
Panner disease
Panner disease is an osteonchondrosis that affects the capitellum in throwing athletes between the ages of 7 and 12 years, who present with pain and impaired extension of the dominant arm.12,58,59 Panner disease is thought to occur because of disruption of the tenuous vascular supply to the capitellum. Early in Panner disease, radiographic subchondral lucency may be appreciated, whereas disease progression may demonstrate a fragmented and sclerotic capitellum.12,58,59 In contradistinction to osteochondritis dissecans, Panner disease is rarely associated with intra-articular bodies and characteristically responds to conservative management. Once healed, there is usually no residual radiographic abnormality.12,59 Low T1 and high T2 signal in the capitellum is typical on MRI in the acute setting, whereas low T2-weighted signal may develop in the setting of sclerosis and healing.59
Osteochondritis dissecans
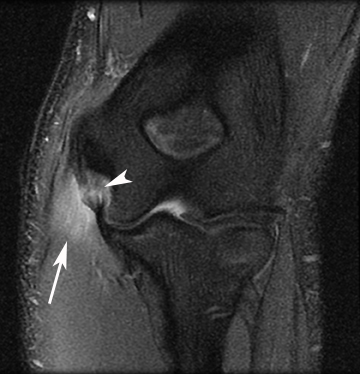
Osteochondritis dissecans of the capitellum usually affects adolescent athletes between 12 and 16 years old.12,60,61 Lesions are typically unilateral in baseball pitchers, handball and water polo players, but bilateral in gymnasts and weightlifters.62 Patients typically present with pain, stiffness, and swelling. Radiographs may be normal early in the disease, but will eventually show capitellar lucency and articular flattening; sclerosis, fragmentation, loose bodies, and radial head enlargement occur later.60-62 MRI is more sensitive for detecting early osteochondral injury and should be obtained if there is any suspicion of defect on initial imaging. Early osteochondritis demonstrates low T1-weighted signal in the capitellum, with or without high T2 signal.25 Injury to the subchondral bone occurs early, and may progress to separation of the articular cartilage with fragmentation in lesions classified as unstable.12,25,60 Fragment instability is implied by any of the following: high T2 signal surrounding the fragment, cysts deep to the fragment, or high T2 signal within the fragment.12,25,60 MR arthrography can help detect cartilage defects and intra-articular bodies, and can help guide management decisions (Figure 12).12,61,62 Type I (nondisplaced) lesions respond to rest, non-steroidal anti-inflammatory drugs (NSAIDs), and physical therapy.58 Type II (mildly displaced) fragments are treated with splinting and rest, while Type III (detached) fragments require surgical intervention.12, 61, 62 If left untreated, fragment migration with progressive joint debility may result.12,24
Elbow dislocation
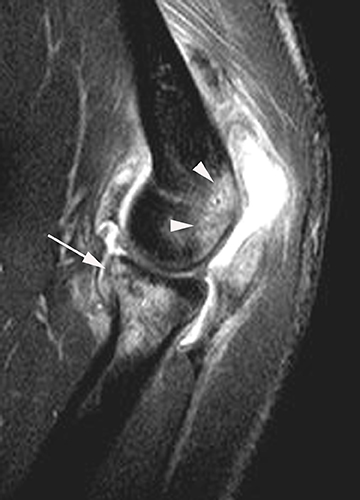
The elbow is the second-most commonly dislocated joint, with posterior dislocation being the most common type.63 The ulna is displaced posteriorly relative to the humerus, resulting in impaction of the coronoid process against olecranon and posterior capitellum against the radial head (Figure 13). When dislocations are associated with coronoid process and radial head fractures, the injury pattern is referred to as the “terrible triad.”64,65 The radial and ulnar collateral ligament complexes are almost always ruptured after elbow dislocation, and MRI is not necessary for confirmation. However, if MRI is performed after elbow dislocation, the adjacent neurovascular structures should be evaluated, given the morbidity associated with these lesions.66
Conclusion
Imaging plays an important role in the evaluation of athletes with elbow soft tissue and/or osseous trauma. Tendinosis and tendon tears of the common extensor tendon origin occurring in tennis players are far more common than injuries involving the common flexor-pronator tendon origin of golfers and pitchers. Concomitant lateral and medial collateral ligament injuries should be sought with MR imaging or sonography in patients with recalcitrant elbow pain in order to address underlying sources of instability. Finally, pitching injuries related to medial tension overload, lateral compression and extension overload include injuries of the flexor-pronator tendon and lateral collateral ligament complex, cubital tunnel syndrome, medial epicondyle apophysitis and avulsion injuries, sublime tubercle and olecranon stress fractures, posteromedial impingement, Panner disease and osteochondritis dissecans.
References
- Stevens KJ, McNally EG. Magnetic resonance imaging of the elbow in athletes. Clin Sports Med. 2010;29(4):521-553.
- Davis KW. Imaging pediatric sports injuries: upper extremity. Radiol Clin North Am. 2010;48:1199-1211.
- Anderson MW, Alford BA. Overhead throwing injuries of the shoulder and elbow. Radiol Clin North Am. 2010;48(6):1137-1154.
- Kijowski R, Tuite MJ. Pediatric throwing injuries of the elbow. Semin Musculoskelet Radiol. 2010;14(4):419-429.
- Goergen T, Dalinka MK, Alazraki N et al. Chronic elbow pain. American College of Radiology. ACR Appropriateness Criteria. Radiology. 2000;215 suppl:339-343.
- Lin J, Jacobson JA, Fessell DP, et al. An illustrated tutorial of musculoskeletal sonography: part 2, upper extremity. AJR Am J Roentgenol. 2000;175(4):1071-1079.
- Frick MA, Murthy NS. Imaging of the elbow: muscle and tendon injuries. Semin Musculoskelet Radiol. 2010;14(4):430-437.
- Delport A, Zoga A. MR and CT arthrography of the elbow. Semin Musculoskelet Radiol. 2012;16:15-26.
- Abrams GD, Stoller DW, Safran MR. MRI and arthroscopy correlations of the elbow: a case-based approach. Instr Course Lect. 2012;61:235-249.
- Wenzke DR. MR imaging of the elbow in the injured athlete. Radiol Clin North Am. 2013;51:195-213.
- Lomasney LM, Choi H, Jayanthi N. Magnetic resonance arthrography of the upper extremity. Radiol Clin North Am. 2013;51(2):227-237.
- Simonson S, Lott K, Major NM. Magnetic resonance imaging of the elbow. Semin Roentgenol. 2010;45(3):180-193.
- Kotnis NA, Chiavaras MM, Harish S. Lateral epicondylitis and beyond: imaging of lateral elbow pain with clinical-radiologic correlation. Skeletal Radiol. 2012;41(4):369-386.
- Bredella MA, Tirman PF, Fritz RC, et al. MR imaging findings of lateral ulnar collateral ligament abnormalities in patients with lateral epicondylitis. AJR Am J Roentgenol. 1999;173(5):1379-1382.
- Struijs PA, Spruyt M, Assendelft WJ, et al. The predictive value of diagnostic sonography for the effectiveness of conservative treatment of tennis elbow. AJR Am J Roentgenol. 2005;185:1113-1138.
- Stenhouse G, Sookur P, Watson M. Do blood growth factors offer additional benefit in refractory epicondylitis? A prospective, randomized pilot trial of dry needling as a stand-alone procedure versus dry needling and autologous conditioned plasma. Skeletal Radiol. 2013;42(11):1515-1520.
- Hayter CL, Adler RS. Injuries of the elbow and the current treatment of tendon disease. AJR Am J Roentgenol. 2012;199(3):546-557.
- Sasaki K, Tamakawa M, Onda K, et al. The detection of the capsular tear at the undersurface of the extensor carpi radialis brevis tendon in chronic tennis elbow: the value of magnetic resonance imaging and computed tomography arthrography. J Shoulder Elbow Surg. 2011;20(3):420-425.
- Walz DM, Newman JS, Konin GP, et al. Epicondylitis: pathogenesis, imaging, and treatment. Radiographics. 2010;30(1):167-184.
- Martin S, Sanchez E. Anatomy and biomechanics of the elbow joint. Semin Musculoskelet Radiol. 2013;17(5):429-436.
- Beltran LS, Bencardino JT, Beltran J. Imaging of sports ligamentous injuries of the elbow. Semin Musculoskelet Radiol. 2013;17(5):455-465.
- Giannicola G, Polimanti D, Sacchetti FM, et al. Soft tissue constraint injuries in complex elbow instability: surgical techniques and clinical outcomes. Orthopedics. 2012;35(12):e1746-1753.
- Konin GP, Nazarian LN, Walz DM. US of the elbow: indications, technique, normal anatomy, and pathologic conditions. Radiographics. 2013;33(4):E125-147.
- Patten RM. Overuse syndromes and injuries involving the elbow: MR imaging findings. AJR Am J Roentgenol. 1995;164(5):1205-1211.
- Hayter CL, Giuffre BM. Overuse and traumatic injuries of the elbow. Magn Reson Imaging Clin N Am. 2009;17(4):617-638, v.
- Gaary EA, Potter HG, Altchek DW. Medial elbow pain in the throwing athlete: MR imaging evaluation. AJR Am J Roentgenol. 1997;168(3):795-800.
- Murthi AM, Keener JD, Armstrong AD, et al. The recurrent unstable elbow: diagnosis and treatment. Instr Course Lect. 2011;60:215-226.
- Hariri S, Safran MR. Ulnar collateral ligament injury in the overhead athlete. Clin Sports Med. 2010;29(4):619-644.
- Kim NR, Moon SG, Ko SM, et al. MR imaging of ulnar collateral ligament injury in baseball players: Value for predicting rehabilitation outcome. Eur J Radiol. 2011;80(3):e422-426.
- Schwartz ML, Thornton DD, Larrison MC, et al. Avulsion of the medial epicondyle after ulnar collateral ligament reconstruction: imaging of a rare throwing injury. AJR Am J Roentgenol. 2008;190(3): 595-598.
- Wear SA, Thornton DD, Schwartz ML, et al. MRI of the reconstructed ulnar collateral ligament. AJR Am J Roentgenol. 2011;197(5):1198-1204.
- Glajchen N, Schwartz ML, Andrews JR, et al. Avulsion fracture of the sublime tubercle of the ulna: a newly recognized injury in the throwing athlete. AJR Am J Roentgenol. 1998;170(3):627-628.
- Grumet RC, Friel NA, Cole BJ. Bony avulsion of the medial ulnar collateral ligament in a gymnast: a case report. J Shoulder Elbow Surg. 2010;19(7):e1-6.
- Stevens K, Kwak A, Poplawski S. The biceps muscle from shoulder to elbow. Semin Musculoskelet Radiol. 2012;16(4):296-315.
- Giuffrè BM, Moss MJ. Optimal positioning for MRI of the distal biceps brachii tendon: flexed abducted supinated view. AJR Am J Roentgenol. 2004;182(4):944-946.
- Miller TT, Adler RS. Sonography of tears of the distal biceps tendon. AJR Am J Roentgenol. 2000;175(4):1081-1086.
- Nho SJ, Strauss EJ, Lenart BA, et al. Long head of the biceps tendinopathy: diagnosis and management. J Am Acad Orthop Surg. 2010;18(11):645-656.
- Blease S, Stoller DW, Safran MR, et al. The elbow. In: Stoller DW, ed. Magnetic resonance imaging in orthopedics and sports medicine. 3rd ed. Baltimore, MD: Lippincott Williams & Wilkins; 2007:1463-1626.
- Dirim B, Brouha SS, Pretterklieber ML, et al. Terminal bifurcation of the biceps brachii muscle and tendon: anatomic considerations and clinical implications. AJR Am J Roentgenol. 2008;191:W248-255.
- Brigido MK, De Maeseneer M, Morag Y. Distal biceps brachii. Semin Musculoskelet Radiol. 2013;17(1):20-27.
- Koplas MC, Schneider E, Sundaram M. Prevalence of triceps tendon tears on MRI of the elbow and clinical correlation. Skeletal Radiol. 2011;40(5): 587-594.
- Van wagenberg JM, Turkenburg JL, Rahusen FT. et al. The posterior transtriceps approach for intra-articular elbow diagnostics, definitely not forgotten. Skeletal Radiol. 2013;42(1):55-59.
- Tagliafico A, Gandolfo N, Michaud J, et al. Ultrasound demonstration of distal triceps tendon tears. Eur J Radiol. 2012;81(6):1207-1210.
- Yoon MY, Koris MJ, Ortiz JA, et al. Triceps avulsion, radial head fracture, and medial collateral ligament rupture about the elbow: a report of 4 cases. J Shoulder Elbow Surg. 2012;21(2):e12-17.
- Kim JY, Lee JS, Kim MK. Fractures of the capitellum concomitant with avulsion fractures of the triceps tendon. J Hand Surg Am. 2013;38(3):495-497.
- Floemer F, Morrison WB, Bongartz G, et al. MRI characteristics of olecranon bursitis. AJR Am J Roentgenol. 2004;183(1):29-34.
- Shell D, Perkins R, Cosgarea A. Septic olecranon bursitis: recognition and treatment. J Am Board Fam Pract. 1995;8(3):217-220.
- Stell IM. Septic and non-septic olecranon bursitis in the accident and emergency department--an approach to management. J Accid Emerg Med. 1996;13(5):351-353.
- Hash TW, Bogner EA. Nerve entrapment and compression syndromes of the elbow. Semin Musculoskeletal Radiol. 2010;14(4):438-448.
- Li X, Dines JS, Gorman M, et al. Anconeus epitrochlearis as a source of medial elbow pain in baseball pitchers. Orthopedics. 2012;35(7):e1129-1132.
- Cohen SB, Valko A, Zoga A, et al. Posteromedial elbow impingement: Magnetic resonance imaging findings in overhead throwing athletes and results of arthroscopic treatment. Arthroscopy. 2011:27;1364-1370.
- Patel NB, Thomas S, Lazarus ML. Throwing injuries of the upper extremity. Radiol Clin North Am. 2013;51(2):257-277.
- Harada M, Takahara M, Sasaki J, et al. Using sonography for the early detection of elbow injuries among young baseball players. AJR Am J Roentgenol. 2006;187(6):1436-1441.
- Wei AS, Khana S, Limpisvasti O, et al. Clinical and magnetic resonance imaging findings associated with Little League elbow. J Pediatr Orthop. 2010;30(7):715-719.
- Blake JJ, Block JJ, Hannah GA, et al. Unusual stress fracture in an adolescent baseball pitcher affecting the trochlear groove of the olecranon. Pediatr Radiol. 2008;38(7):788–790.
- Sheehan SE, Dyer GS, Sodisckson et al. Traumatic elbow injuries: What the orthopedic surgeon wants to know. Radiographics. 2013;33(3):869-888.
- Rauck RC, Lamont LE, Doyle SM. Pediatric upper extremity stress injuries. Curr Opin Pediatr. 2013;25(1):40-45.
- Iyer RS, Thapa MM, Khanna PC, et al. Pediatric bone imaging: imaging elbow trauma in children--a review of acute and chronic injuries. AJR Am J Roentgenol. 2012;198(5):1053-1068.
- Dwek JR, Chung CB. A systematic method for evaluation of pediatric sports injuries of the elbow. Pediatr Radiol. 2013;43 Suppl 1:S120-128.
- Baker CL, Romeo AA, Baker CL. Osteochondritis dissecans of the capitellum. Am J Sports Med. 2010;38(9):1917-1928.
- Zellner B, May MM. Elbow injuries in the young athlete – an orthopedic perspective. Pediatr Radiol. 2013;43 suppl:129-134.
- Bancroft LW, Pettis C, Wasyliw C et al. Osteochondral lesions of the elbow. Semin Musculoskelet Radiol. 2013 Nov;17(5):446-454.
- Schaeffeler C, Waldt S, Woertler K. Traumatic instability of the elbow - anatomy, pathomechanisms and presentation on imaging. Eur Radiol. 2013;23(9):2582-2593.
- Rosas HG, Lee KS. Imaging acute trauma of the elbow. Semin Musculoskelet Radiol. 2010;14:394-411.
- Reichel LM, Milam GS, Hillin CD, et al. Osteology of the coronoid process with clinical correlation to coronoid fractures in terrible triad injuries. K Shoulder Elbow Surg. 2013;22(3):323-328.
- Carter SJ, Germann CA, Dacus AA, et al. Orthopedic pitfalls in the ED: neurovascular injury associated with posterior elbow dislocations. Am J Emerg Med. 2010;28(8):960-965.