Imaging of the mediastinum in oncology











Dr. Lesslie was a Radiology Resident at the University of Texas Health Science Center Medical School at the time of this submission and is currently a radiologist with Greater Houston Radiology Associates. Dr. Chasen is a Professor, the Department Chairman ad interim of the Department of Radiology, Division of Diagnostic Imaging, The University of Texas M.D. Anderson Cancer Center. Dr. Munden is a Professor, the Associate Division Head of Translational and Clinical Research, and the Section Chief of Thoracic Imaging, Division of Diagnostic Imaging, The University of Texas M.D. Anderson Cancer Center, Houston, TX.
The mediastinum is composed of various structures within the central portion of the thorax that are bounded by the lungs, the diaphragm, and the thoracic inlet. Because of this wide variety of anatomic structures, mediastinal tumors constitute a heterogeneous group of neoplasms, both primary and metastatic. Detection of mediastinal abnormalities requires familiarity with the chest radiograph, as most mediastinal tumors are discovered in asymptomatic patients on routine chest radiography. Once a mediastinal abnormality is detected by a chest radiograph, further radiologic evaluation involves cross-sectional imaging with computed tomography (CT) or magnetic resonance imaging (MRI) and may employ other imaging techniques, such as positron emission tomography (PET) or integrated PET/CT. This article will review fundamental radiologic findings of mediastinal abnormalities on chest radiographs and will address the salient features of mediastinal tumors on other imaging modalities, including CT, MRI, PET, and integrated PET/CT.
Division of the mediastinum
The diagnostic evaluation of mediastinal disease requires a thorough understanding of mediastinal anatomy on chest radiography and cross-sectional imaging. Localizing and understanding the relationship of an abnormality to a mediastinal compartment or normal structure can provide a valuable clue for the diagnosis of a mediastinal mass. The chest radiograph is the most often performed radiographic examination, constituting more than 40% of the total volume of radiographs, with >50 million chest radiographs performed per year in the United States. 1 Therefore, it is important for radiologists to understand the appearance of normal structures and how they can be altered by disease. In particular, the detection of mediastinal disease can be difficult with conventional chest radiographs, as many masses are of soft tissue density and are surrounded by structures composed of soft tissue.
To facilitate the detection and classification of mediastinal lesions, most radiologists divide the mediastinum into 3 compartments, as proposed by Felson 2 (Figure 1). The anterior mediastinum is bounded anteriorly by the sternum and posteriorly by a line drawn from the anterior aspect of the trachea and along the posterior heart border. The posterior mediastinum is defined by a line that is 1 cm posterior to the anterior edge of the vertebral bodies. The middle mediastinal compartment lies between the anterior and posterior mediastinum. This division of mediastinal compartments is also used in cross-sectional imaging.
Lines, stripes, and interfaces
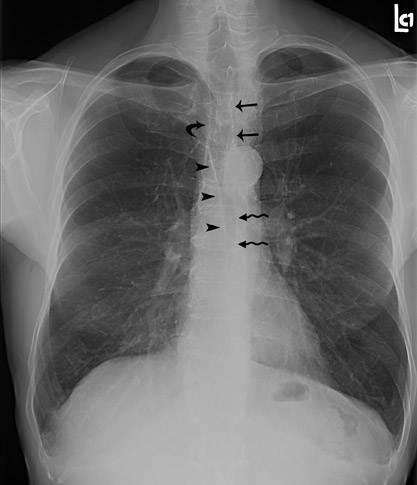
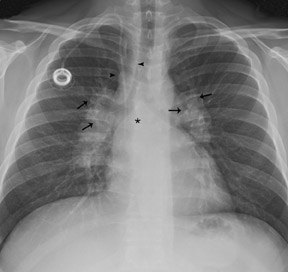
Normal anatomic structures of the mediastinum may be altered by mediastinal disease. This alteration of normal anatomy may alert the radiologist to the presence of a mediastinal mass. Thus, familiarity with the appearance of normal mediastinal structures on chest radiography is a crucial part of identifying an abnormality (Figure 2).
The anterior and posterior junction lines are normal mediastinal structures that are not evident in all patients. However, when present, these lines can be helpful in determining an abnormality. The close apposition of the lungs and pleura anterior to the ascending aorta and right ventricular outflow tract forms the anterior junction line, which courses obliquely from the upper right to lower left behind the retromanubrial region toward the heart. 3 Similarly, the posterior junction line is formed by the close apposition of the lungs and pleura posterior to the esophagus and anterior to the spine, coursing vertically from the lung apices to the top of the aortic arch. 4 These lines should be smooth and concave. Although no abnormality may be assumed in the absence of these landmarks, when either is displaced or bulging, it is an indicator of a possible mediastinal abnormality.
The right paratracheal stripe appears as a thin, soft tissue density structure located between the tracheal air column and the adjacent right lung. 5 This can be followed as it passes vertically from the undersurface of the clavicles to the azygos arch. It should be smooth and range in width from 1 to 4 mm.
The azygoesophageal recess is an interface formed by the apposition of the right lung and pleura and the right lateral margin of the azygos vein and esophagus. This descends vertically from the undersurface of the azygos arch to the diaphragm, with a gentle convexity curving toward the left. The interface should be smooth without focal bulges or extreme deviation from the midline.
The left paraspinal interface is formed where the left lung and pleura abut the left lateral margin of the vertebral bodies and paravertebral soft tissues. Although not always seen in its entirety, it should be smooth as it courses vertically from the level of the aortic knob to the diaphragm and have a uniform distance from the lateral margin of the spine.
Conventional radiographic signs
In addition to altering normal structures, the presence of mediastinal malignancies can result in radiographic signs or patterns that aid in detection and localization. Many of these classic signs and patterns were originally described by Felson 6 and continue to be beneficial in interpreting chest radiographs.
When a mass abuts a normal mediastinal structure of similar radiodensity, the margins of the 2 structures will be obliterated. This sign is referred to as the "silhouette sign," although there is actually desilhouetting of the normal structure by the mass. This apparent loss of the margin of the normal structure can be used to localize a mediastinal mass to the same compartment as the normal structure.
The hilar overlay sign (Figure 3) is another sign described by Felson 6 that is especially useful in distinguishing an anterior mediastinal mass from a prominent cardiac silhouette. If the bifurcation of the main pulmonary artery is >1 cm medial to the lateral border of the cardiac silhouette, it is strongly suggestive of a mediastinal mass. If the pulmonary artery arises from the lateral heart border, this favors an enlarged heart. In other words, because the pulmonary arteries arise from the heart, when the heart enlarges, then pulmonary arteries must move laterally with the heart border. An anterior mediastinal mass that appears as an enlarged cardiac silhouette will not cause displacement of the pulmonary arteries.
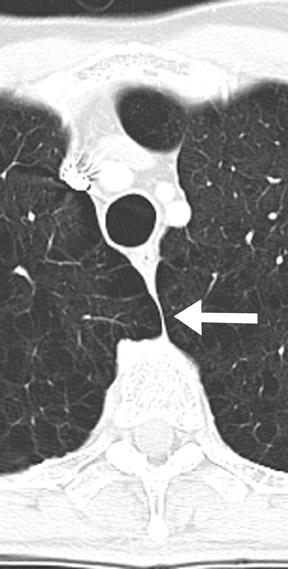
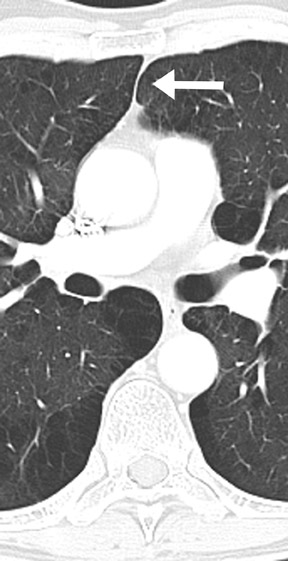
The hilar convergence sign is used to distinguish between a prominent hilum and an enlarged pulmonary artery. 6 If the pulmonary arteries converge into the lateral border of a hilar mass, the mass represents an enlarged pulmonary artery (Figure 4). If the convergence appears behind the abnormality or arises from the heart, a mediastinal mass is more likely. In other words, because the pulmonary artery branches arise from the main pulmonary artery trunk, an enlarged pulmonary artery will have branches that arise from its outer margin (the vessels converge toward the main pulmonary artery). A hilar mass may have the appearance of an enlarged pulmonary artery, but the vessels will not arise from the margin; instead they will seem to pass through the margins as they converge on the true artery (Figure 5).
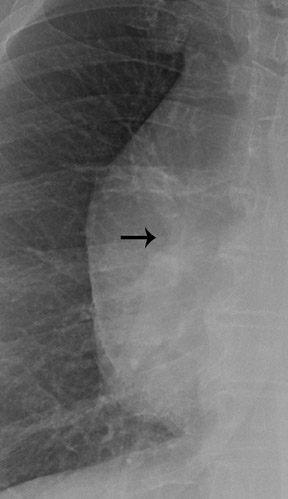
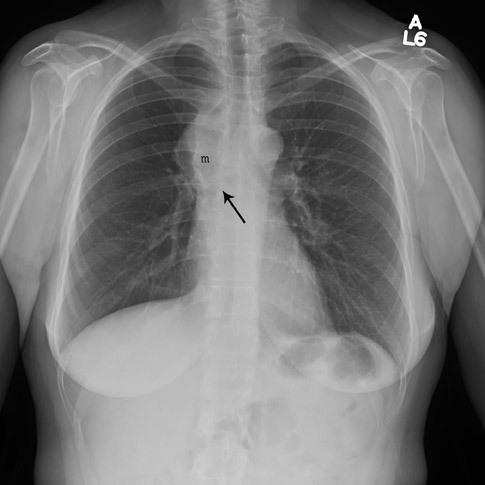
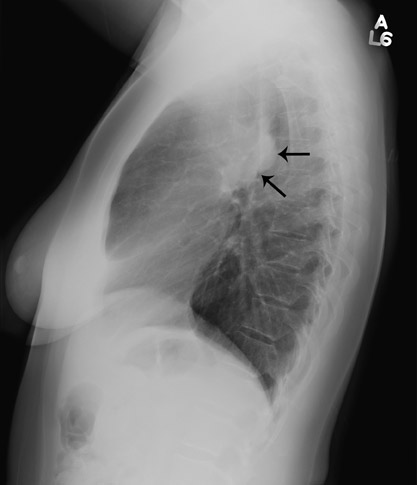
Finally, the cervicothoracic sign (Figure 6) is used to determine the location of a mediastinal lesion in the upper chest. The uppermost border of the anterior mediastinum ends at the level of the clavicles. However, the medial and posterior mediastinum extends above the clavicles. A mediastinal mass that projects superior to the level of the clavicles must therefore be located either within the middle or posterior mediastinum. Furthermore, the more cephalad the mass extends, the more posterior the location. 6
Once an abnormality is detected on a conventional chest radiograph, cross-sectional imaging plays an important role in the further characterization of the mediastinal mass. CT and MRI provide excellent anatomic definition and characterization of mediastinal masses and, therefore, are the imaging modalities of choice. More recently, functional imaging, using PET and integrated PET/CT imaging, has been useful in assessing mediastinal masses. 7
Tumors of the anterior mediastinum
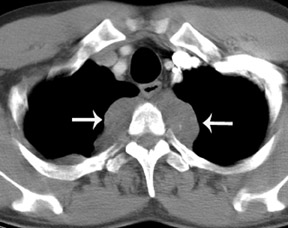
The most common primary tumor of the anterior mediastinum is thymoma. 8 Thymoma usually occurs as an incidental finding in an otherwise healthy individual but may also present along with a parathymic syndrome, such as myasthenia gravis, pure red cell aplasia, and hypogammaglobulinemia. Thymoma is characteristically a well-defined, round or oval anterior mediastinal mass arising from one of the thymic lobes (Figure 7). They are typically located just anterior to the aortic root, although they can occur anywhere from the neck to the cardiophrenic angle. On CT, thymoma presents as an encapsulated, well-defined soft tissue mass that may be homogeneous or heterogeneous depending upon the degree of hemorrhage, necrosis, or cyst formation. Calcifications are infrequent and may be small, curvilinear, or punctuate. On MRI, a thymoma may be homogeneous or heterogeneous in signal, but usually appears isointense to muscle on T1-weighted imaging and has increased signal on T2-weighted imaging. Invasive thymomas spread locally by seeding the pleural space and may even progress to circumferentially encase the lung. 9 The invasive nature is usually not determined by imaging, but pleural or pericardial implants can occasionally be detected by CT and MRI. MRI can also be utilized to reveal involvement of vascular structures. 10
Thymic carcinoma is an aggressive malignancy with a propensity to spread through early local invasion to regional lymph nodes and with distant metastases. 11,12 CT shows a large, poorly defined, infiltrative anterior mediastinal mass that may exhibit cystic changes. 13 Pleural and pericardial effusions are frequently associated, in contrast to benign or invasive thymoma, which rarely are associated with pleural effusions. 13 Thymic carcinoma can be difficult to differentiate from thymoma in the absence of distant metastases. 8
Thymic carcinoid is a rare malignancy arising from the thymic cells of neural crest origin. Patients often present with endocrine abnormalities, most commonly Cushing's syndrome or multiple endocrine neoplasia type 1 (MEN 1) syndrome. CT shows a large, lobulated anterior mediastinal mass that may have foci of hemorrhage and necrosis. Calcification may also be present. 12
Mediastinal germ cell tumors are thought to originate from primitive germ cells misplaced in the mediastinum during early embryogenesis. 14 The most common extragonadal primary site is the anterior mediastinum, especially the anterosuperior portion. 15,16 Teratomas are the most common mediastinal germ cell tumors. 15,16 Mature teratomas, which represent approximately 60% to 70% of mediastinal germ cell tumors, are usually well-differentiated and benign. 16 On chest radiography, these are rounded to lobulated, well-defined anterior mediastinal masses that may extend to one side of the midline and may attain large sizes. 17 Calcification and, rarely, identifiable bone or teeth, may be evident. 17 CT reveals a heterogeneous, predominantly cystic mass with well-defined margins. An anterior mediastinal mass with foci of fluid, soft tissue, calcium, and/or fat attenuation is highly specific for a mature teratoma.
Most lesions of the thyroid are goiters or cysts, and it is not uncommon for them to be detected on CT. Thyroid lesions are reported to extend into the mediastinum in 1% to 3% of patients at the time of thyroidectomy. 18 The most important feature to distinguish mediastinal thyroid from other disease is continuity between the cervical and mediastinal components. While most thyroid lesions extending into the mediastinum are goiters, radiologists must be aware that malignant lesions can also present in this manner. The most common histologies of thyroid carcinomas are papillary, follicular, medullary, anaplastic, and Hürthle cell. 19 Of these, medullary carcinoma is the most likely to metastasize to the mediastinum, while the others tend to spread to the lungs. CT complements nuclear medicine imaging of thyroid malignancies by showing anatomical definition of a primary tumor, extent of mediastinal involvement, and pulmonary metastases. Because of the high iodine content of thyroid tissue, unenhanced CT imaging of the thyroid may reveal foci of high attenuation. There may also be areas of low attenuation due to hemorrhage and cyst formation, and calcifications may be present. Intravenous contrast is usually not administered because of interference with radioactive iodine nuclear medicine studies. However, if contrast is administered, intense and prolonged enhancement may occur. Radioactive Iodine-123 and -131 scintigraphy may be confirmatory when radioactive uptake from functioning thyroid tissue is exhibited.
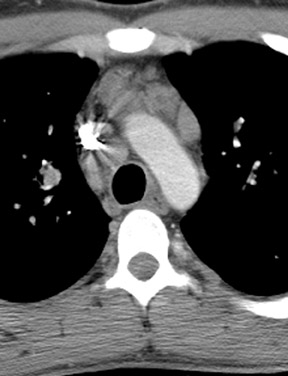
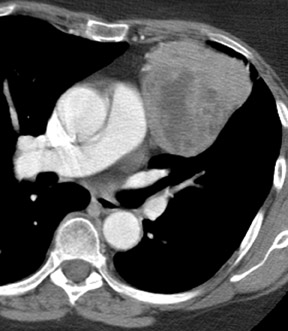
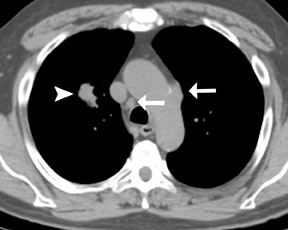
Primary cardiac neoplasms are rare, with a reported prevalence of only 0.001% to 0.03% of patients in an autopsy series. 20 The most common primary cardiac tumor is myxoma, which comprises approximately half of all cases. 20 Cardiac sarcoma is the second most common primary cardiac neoplasm. Although still relatively uncommon, cardiac involvement by metastatic disease is estimated to be 100 to 1000 times more common than a primary cardiac neoplasm. 21 Cardiac metastasis is typically associated with widely disseminated disease. The most frequently implicated primary neoplasms are lung, breast, lymphoma, and melanoma. 22 Echocardiography has traditionally been the primary imaging modality for intracardiac disease. However, the morphology and location of a cardiac tumor can be adequately shown by CT. With the development of multichannel CT and cardiac-gated CT, imaging of the heart with CT is a rapidly emerging technology that may prove useful in imaging cardiac tumors. In addition, CT is superior to echocardiography in the evaluation of the pericardium, great vessels, and other mediastinal structures, which allows for the assessment of disease extent. 21 Cardiac-gated MRI has a well-established role in the evaluation of a cardiac mass 21 and is currently the imaging modality of choice for cardiac tumors. The advantages of MRI include a wide field of view, high contrast and spatial resolution, and multiplanar imaging. These features provide accurate localization of a mass, including its anatomic relationship to the cardiac chambers (Figure 8). MRI also allows determination of involvement of myocardium, pericardium, or other adjacent mediastinal structures. Gadolinium contrast administration may show differential enhancement of a tumor in comparison to the surrounding normal myocardium. 21
Lymphoma is another malignancy that is well known to affect the anterior mediastinum, although it may be present in any of the 3 mediastinal compartments. This entity will be discussed within the next section.
Tumors of the middle mediastinum
Most middle mediastinal tumors are mainly lymphatic in origin, including lymphoma and metastatic tumors, especially in the lung and breast. Also, esophageal cancer can occur as a primary malignancy of the middle mediastinum (Figure 9). However, both lymphoma and metastatic disease may be found in any of the mediastinal compartments.
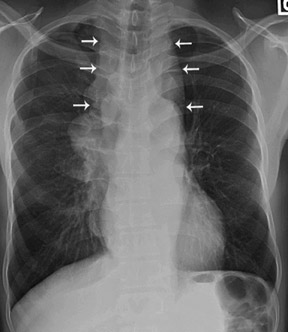
Lymphoma is one of the most common mediastinal neoplasms. The 2 major classifications, Hodgkin's disease (HD) and non-Hodgkin's lymphoma (NHL), both may affect the mediastinum. Typically, HD involves the mediastinum, whereas NHL involves the lungs; but with extensive or disseminated disease, there may be an overlap between both regions. The majority of patients with HD have an abnormal chest radiograph, while less than half of patients with NHL have abnormalities on chest radiography. 23 On CT, both mediastinal HD and NHL may present as multiple, rounded soft tissue masses that correspond to individual lymph nodes or as a bulky soft tissue mass due to coalescence of lymphadenopathy. Homogeneous soft tissue attenuation is typical, although heterogeneity with areas of low attenuation may be present, which represent necrosis, hemorrhage, or cyst formation. Calcification is rare in untreated patients. CT may reveal associated mediastinal infiltration and displacement, compression, or invasion of the airway and/or vascular structures, such as the superior vena cava (SVC), the pericardium, and the heart. Involvement of the pleura, lung, and chest wall may also be seen. 23 Accurate staging of lymphoma can result in improvement in patient outcomes, as disease extent is an important factor in determining appropriate therapy. Contrast-enhanced CT is currently the standard imaging procedure for the staging and restaging of lymphoma. Lymph node involvement by CT is defined by size criteria, with 10 mm measured in the short-axis plane considered the upper limit of normal. This is problematic, as small lymph nodes harboring active disease may be overlooked on CT, while benign, inflammatory lymphadenopathy may be misdiagnosed as lymphoma. Several studies have shown the value of 18-fluorodeoxyglucose PET (FDG-18-PET) in the baseline evaluation of lymphoma 24-28 ; and FDG-PET has also been shown to be superior to CT for the staging of lymphoma. 24,27-29 Another useful application of FDG-PET is the assessment of disease response after treatment (restaging), where active disease can be differentiated from fibrotic tissue in residual masses identified by CT. 30-33 There is also data that establishes the ability of FDG-PET to determine a prognosis. A negative PET scan obtained after treatment has been shown to predict a low risk of relapse and longer progression-free survival compared with positive PET results. 34-36
Esophageal carcinomas most commonly involve the distal esophagus and are of adenocarcinoma histology, usually in the setting of pre-existing Barrett's esophagus. These aggressive malignancies are often associated with a dismal prognosis, with surgery alone resulting in a survival rate of only 6% to 40% at 9 to 24 months. 37 Multimodality therapy has been shown to improve survival in a certain subset of patients 37 ; therefore, accurate staging is essential to guide treatment planning and identify patients who may benefit from multimodality therapy. Traditional noninvasive staging modalities include CT, endoscopic ultrasonography (EUS), and FDG-PET. Endoscopic ultrasonography is useful for the evaluation of the depth of primary tumor penetration within the wall and invasion of periesophageal tissues. Endoscopic ultrasonography has a reported accuracy for determining T and N staging of 85% and 75%, respectively, and a sensitivity ranging from 85% to 95% and 70% to 80%, respectively. 38 However, staging by EUS is not possible in all patients with esophageal cancer because of esophageal stenosis or obstruction by tumor. Endoscopic ultrasonography is also limited for staging distant metastases. In addition to evaluation of the primary tumor, compared with EUS, CT has an additional benefit in the evaluation of mediastinal invasion, spread to lymph nodes, and distant metastases. Metastatic disease typically involves distant lymph nodes (usually abdominal), liver, and lung. Assessment of the primary tumor with CT is limited without contrast distension of the esophagus, but may be useful in assessing response to therapy. 37 It has been shown that FDG-PET is more effective than CT in detecting distant metastases. 38 This is an important advantage, as the identification of patients with distant metastatic disease avoids unnecessary surgery and ineffective radical therapies that may be associated with high morbidity in patients with incurable disease. In fact, the recognition of local or distant metastases with FDG-PET has been shown to be highly predictive of survival. 37 Recently, FDG-PET has also been shown to be an accurate test to predict long-term survival after preoperative chemoradiation therapy (CRT), with a post-CRT FDG-PET standard uptake value (SUV) of ≥4 associated with a significantly worse 2-year survival rate than those with an SUV of <4. 37 This could assist in customizing therapeutic regimens that minimize futile treatment associated with high morbidity while maximizing therapeutic benefit.
In non-small-cell lung cancer (NSCLC), the presence of mediastinal adenopathy critically impacts treatment planning and potential disease resectability. Ipsilateral mediastinal or subcarinal adenopathy constitutes N2 disease and may be resectable. Contralateral mediastinal adenopathy, ipsilateral scalene, or supraclavicular adenopathy indicate N3 disease, which is nonresectable. Lymph node size on chest CT is the most common criterion for the identification of abnormal lymph nodes, with a short-axis nodal diameter of 10 mm, which is generally considered the upper limit of normal. 39,40 Unfortunately, CT may commonly overestimate or underestimate disease extent within the mediastinum. Imaging with FDG-PET has been shown to be useful in the detection of nodal disease. In a meta-analysis of nodal staging comparing PET and CT, the mean sensitivity and specificity of PET was 79% and 91%, respectively, compared with 60% and 77% for CT, respectively. 41
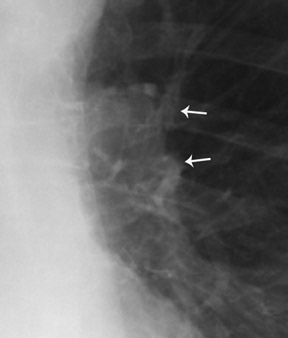
Similar usefulness of PET has been shown for nodal staging in patients with breast cancer. Metastatic spread to the mediastinal lymph nodes commonly occurs in patients with breast cancer. 42 The failure to recognize mediastinal disease may lead to treatment failure and/or the development of distant metastatic disease in patients diagnosed with only locoregional disease by conventional imaging modalities. In a study of 33 patients with advanced breast cancer who underwent both FDG-PET and CT as part of their diagnostic evaluation as well as confirmation by biopsy or follow-up imaging, the sensitivity, specificity, and accuracy for identification of nodal disease by FDG-PET was 85%, 90%, and 88%, respectively, compared with 54%, 85%, and 73%, respectively, by prospective interpretation with CT. 42
Integrated PET/CT represents an exciting advance in FDG-PET imaging, as it offers improved anatomic resolution of FDG-avid lesions. Integrated PET/CT has been shown to be more accurate than either PET or CT alone in tumor staging in NSCLC 7,43 (Figure 10). In a recent study comparing PET, CT, and fused PET/CT, the reported accuracy for detecting metastatic mediastinal lymph nodes was 63% for CT alone, 89% for PET alone, and 93% for PET/CT. Sensitivity and specificity for PET/CT was 89% and 94%, for PET 89% and 89%, and CT 70% and 59%. 7 Similar results have been reported for the use of PET/CT in the staging and restaging of lymphoma. A recent study by Schaefer et al 29 was performed comparing fused PET/CT with contrast-enhanced CT in 60 patients with HD or NHL. The sensitivity of PET/CT and contrast-enhanced CT was 94% and 88%, and the specificity was 100% and 88%, respectively. The promising technology of fused PET/CT in lung carcinoma, esophageal carcinoma, and lymphoma will lead to further utilization in other mediastinal diseases.
Tumors of the posterior mediastinum
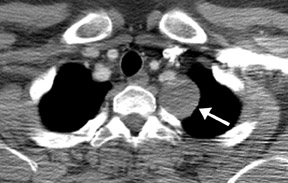
Neurogenic tumors constitute the majority of posterior mediastinal mass lesions 23 (Figure 11). Neurogenic tumors are generally categorized as arising from either peripheral nerves or sympathetic ganglia. Schwannoma, neurofibroma, and malignant tumor of nerve sheath origin arise from peripheral nerves. Ganglioneuroma, ganglioneuroblastoma, and neuroblastoma arise from sympathetic ganglia.
Schwannomas and neurofibromas are the most common mediastinal neurogenic tumors. 23 The malignant counterpart to these benign tumors is the malignant tumor of nerve sheath origin (MTNSO). These tumors usually present as lobulated, spherical paraspinal masses. On cross-sectional imaging, neurofibromas are usually sharply marginated, homogeneous, nonencapsulated lesions. On CT, schwannomas are frequently heterogeneous with areas of low attenuation that correspond to areas of cystic degeneration, hypocellularity, hemorrhage, lipid, or myelin. Punctate calcifications may also be detected on CT. Both types of tumors may display homogeneous, heterogeneous, or peripheral enhancement following intravenous contrast administration. Roughly 10% of schwannomas and neurofibromas grow through the adjacent intervertebral foramen and extend into the spinal canal with a "dumb-bell" or "hourglass" configuration. Malignant tumors of nerve sheath origin may invade adjacent chest wall or mediastinal structures. MRI is indicated in all patients with a possible neurogenic tumor to ex-clude intraspinal tumor extension. MRI typically exhibits low-to-intermediate signal intensity on T1-weighted imaging and may show areas of intermediate-to-high signal intensity on T2-weighted imaging. 14,23
The sympathetic ganglia tumors usually affect children and young adults and include neuroblastoma, ganglioneuro-blastoma, and ganglioneuroma. These tumors originate from the nerve cells, as opposed to the nerve sheaths. Ganglioneuroma and ganglioneuroblastoma typically occur in the posterior mediastinum. On CT, ganglioneuroma may present as a well-marginated, elongated, homogeneous or heterogeneous, paraspinal mass. MRI is useful to accurately define the presence and degree of intra-spinal extension. Homogeneous, intermediate signal intensity may be seen on all sequences. Occasionally, there may be a whorled appearance on T1-weighted images and heterogeneous high signal intensity on T2weighted images. 14,23
Neuroblastomas are typically found in young children. Approximately 50% arise within the adrenal gland, with the mediastinum being the most common extra-abdominal location. When mediastinal in location, neuroblastoma is typically an elongated paraspinal mass. It may displace or invade adjacent structures, cross the midline, and/or cause extensive skeletal erosion. On plain film, calcification may be detected. On CT, calcification is shown in approximately 80% of neuroblastomas. Neuroblastoma is typically heterogeneous on both CT and MRI. MRI may be preferred over CT because of its superior soft tissue contrast and its ability to delineate intraspinal involvement. The lack of ionizing radiation is another advantage, as neuroblastoma is a disease of the pediatric population. MRI exhibits heterogeneous low signal on T1- and high signal on T2weighted imaging. Radionuclide imaging with iodine metaiodobenzylguanidine is indicated for the evaluation of primary and metastatic neuroblastoma. Metaiodobenzylguanidine is an analogue of catecholamine precursors that is relatively specific for tumors of sympathetic origin. 14,23
Conclusion
Mediastinal tumors constitute a wide variety of lesions because of the diverse anatomic structures within the mediastinum. It is important for radiologists to understand normal mediastinal structures, mediastinal compartments, and common mediastinal malignancies in order to detect and characterize mediastinal masses.
