Imaging blunt and penetrating trauma to the neck: Clinical relevance and management
Images

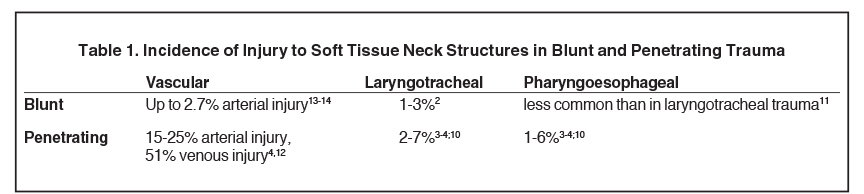
Significant soft tissue trauma to the neck can involve critical upper aerodigestive and cerebrovascular structures whose relatively simple physiologic functions are basic to life support. Fortunately, injury to the neck soft tissues accounts for a relatively small number of trauma resuscitations.1 Not surprisingly, however, the associated morbidity and mortality can he high.1-6 By some reports, laryngotracheal injury in blunt trauma can carry up to 40% mortality.2 Missed pharyngoesophageal perforation carries an associated 20% mortality.7
The aerodigestive and vascular anatomy of the neck is particularly susceptible to injury in direct blunt or penetrating trauma to the anterior neck (Table 1). Additionally, complex and high-impact mechanisms of injuries can compel the neck into extremes of hyperextension, hyperflexion and hyperrotation, subjecting the soft tissue structures to severe shear and tensile forces. Resultant injuries such as laryngotracheal separation and carotid dissections can be devastating. While the presentation is often less dramatic, internal laryngotracheal and pharygoesophageal trauma from foreign body ingestion and instrumentation are comparatively common forms of injury that will likely account for a higher fraction of traumatic neck injuries in centers without Level 1 trauma designation.8-9
Management paradigms in blunt and penetrating neck trauma have evolved over time to increasingly rely on imaging – particularly multidetector computed tomography (MDCT) – to guide surgical, endovascular and medical intervention. The role of the radiologist is therefore increasingly important. This review will discuss the common imaging features and management implications of traumatic injury to the soft tissues of the neck, particularly emphasizing laryngotracheal and pharyngoesophageal injury.
Specific patterns and mechanisms of injury
Although the spectrum of injury from blunt or penetrating trauma to the neck is broad, several identifiable patterns exist which correspond to specific mechanisms of injury.
Strangulation
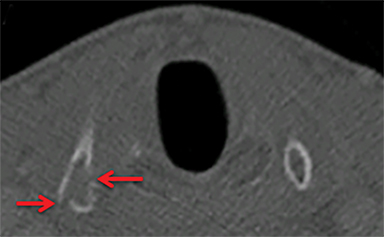
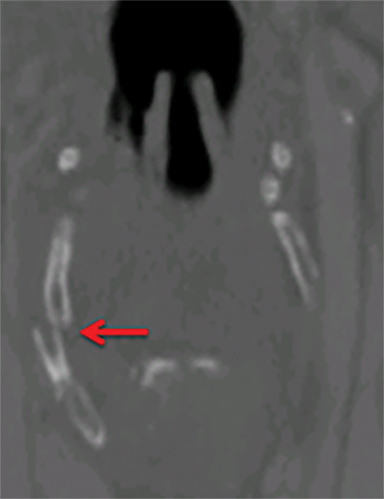
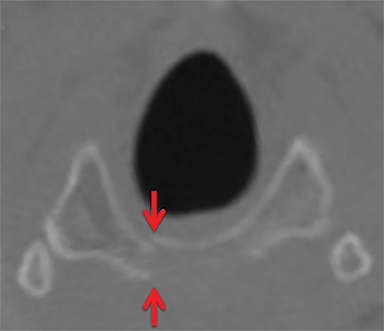
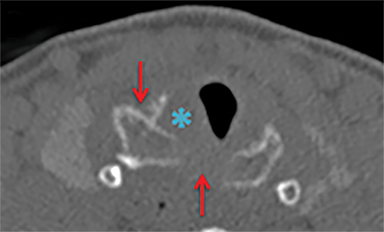
Strangulation injuries, such as from assault or hanging, are associated with characteristic findings that result primarily from crush injuries to the anterior neck against the rigid cervical vertebral bodies. Particular findings include horizontal thyroid cartilage fractures (Figure 1), fractures of the superior thyroid cornua as well as hyoid fractures (Figure 2), malalignment and malposition injuries.15
Hyperextension injury
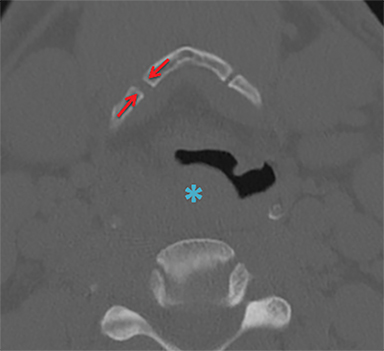
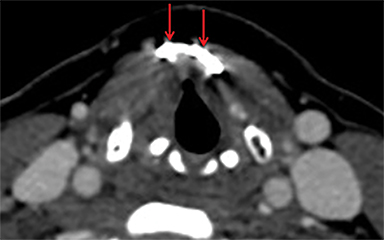
Hyperextension injuries result from shear and tensile forces acting on the aerodigestive structures fixed against the cervical vertebral bodies. Characteristic injuries include tracheal tears, vertical laryngeal (Figure 3) fractures and, in rare cases, complete laryngotracheal separation. Laryngotracheal separation often occurs at the level of the cricoid cartilage, as the airway is comparatively immobile at this location.16
Rapid acceleration and blunt impact (hit from behind)
The so called “padded dashboard” constellation of injuries,16 results from neck hyperextension during rapid acceleration followed by blunt impact of the anterior neck on the car dashboard or steering wheel. This is seen in unrestrained passengers or drivers hit from behind. The injury pattern is that of hyperextension shearing injuries accompanied by crush injuries to the anterior neck.
Pressure against a closed glottis
Rapid increase in intrathoracic or intratracheal pressure against a closed glottis during blunt chest or lower neck impact can result in laryngotracheal rupture. Any component of the subglottic airway can be affected, depending on the level of impact. The prototypical example would be tracheal rupture after rapid deceleration with inappropriately high seat belt position across the lower neck/chest.
Larynx and trachea
Anatomy
The larynx is suspended in the neck via attachments to the hyoid bone superiorly and through fixation inferiorly by the immobile cricoid ring. Extrinsic muscles of the larynx also assist in positioning the larynx in the neck, with attachments to the base of the tongue, mandible, pharynx and sternum.
The myoelastic and aerodynamic properties of the larynx are fundamental to phonation and airway protection. An intact cartilaginous skeleton is the most basic requirement for functionality. Disruption of the endolaryngeal structures including the vocal cord attachments, arytenoid cartilages and mucosal epithelial lining itself also interfere with laryngeal function. Intrinsic muscles of the larynx are also integral to phonation and are innervated by two branches of the vagus nerve, the recurrent laryngeal nerve and the external branch of the superior laryngeal nerve.
Imaging evaluation and management
Simplistically, the larynx can be injured as a result of external – blunt or penetrating – or internal trauma. Internal, or endolaryngeal injury is typically the result of traumatic intubation or, rarely, foreign body ingestion and aspiration. Indications for imaging in the setting of external laryngeal trauma are controversial, but in general imaging should be employed when there is clinical concern for laryngotracheal injury, the airway is stable and the following condition(s) are met:11
- Significant trauma to the anterior neck with or without abnormal physical exam (i.e., dysphonia or hemoptysis).
- Continuity and condition of the endolarynx and trachea not adequately evaluated endoscopically due to hemorrhage or edema.
- Physician is uncertain of extent of laryngeal injury.
- Imaging can be performed under supervision of personnel capable of securing an emergency airway.
Emergent surgical exploration supersedes imaging if the airway is unstable or if the extent of injury clearly warrants immediate operative intervention. In almost all cases where imaging is appropriate, CT is the definitive modality. MRI may add additional value if cartilage fracture is suspected but not confirmed at CT, especially in children or individuals with incompletely ossified cartilages.15
Management of traumatic laryngeal injuries has evolved over time, and newer approaches to operative and nonoperative management will be discussed below.11,16,17
Injuries to the supraglottic larynx
The hyoid bone itself can be malpositioned, indicating disruption of its attachment to the base of tongue and mandible superiorly or of its inferior strap muscle and membranous attachments to the thyroid cartilage and sternum. Hyoid fractures, dislocations and subluxations can occur with blunt trauma, especially strangulation injuries. Particular attention should be paid to the epiglottic petiole as avulsion of the thryoepiglottic membrane is often surgically repaired.18 Definitive diagnosis is made at endoscopy, but hematoma or edema involving the petiole on CT or MRI as well as widening of the pre-epiglottic space can be indicative.
Laryngeal skeletal injuries
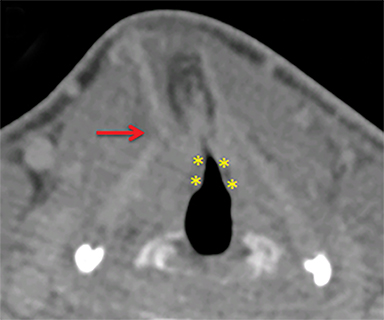
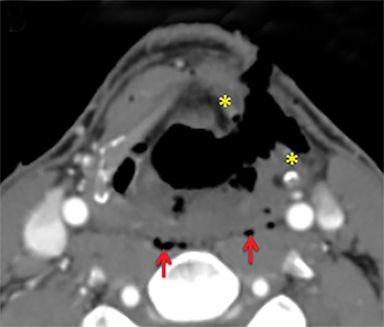
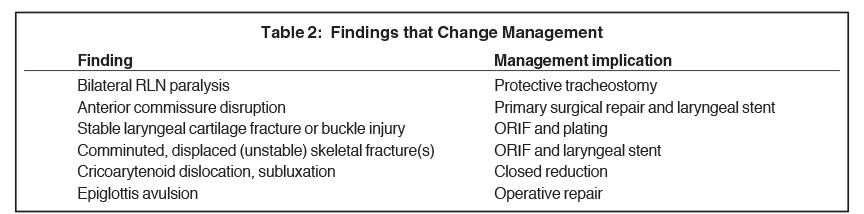
The thyroid and cricoid cartilages can fracture, buckle and dislocate with respect to each other (Figure 4) Paraglottic hemorrhage and/or edema as well as abnormal endolaryngeal contour or configuration are findings at CT that often accompany cartilage injuries (Figure 4) In newer management paradigms, laryngeal cartilage fractures are surgical lesions, reduced and fixed with adaptation plating to restore the skeletal anatomy necessary for proper phonation (Figure 5).11 The surgical approach is informed by whether the fractures are stable (not significantly displaced) and whether there is accompanying endolaryngeal mucosal injury.
If there is high suspicion for cartilaginous injury without a frank fracture line or abnormal contour to the cartilage by CT, MRI may add additional value and is best performed with thin section (2-3mm slice thickness), small field of view and large matrix size (15), preferably at high field strength.
Endolaryngeal injuries
Assessment of the endolaryngeal mucosa and submucosal spaces is important to management decision-making and surgical planning. So-called “reversible” injuries, including submucosal edema/hematoma with intact overlying mucosa as well as minor mucosal lacerations not involving the glottis and without accompanying cartilage fractures, can be treated nonoperatively.16,11 A surgical penetrating endolaryngeal injury is depicted in Figure 6. Disruption of the anterior commissure is of particular importance, as it implies avulsion of the vocal ligaments from the thyroid cartilage. This injury necessitates suturing of the anterior vocal ligament to the thyroid perichondrium to restore the normal scaphoid shape of the glottis (Table 2).11
Arytenoids
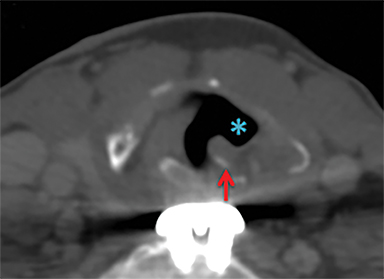
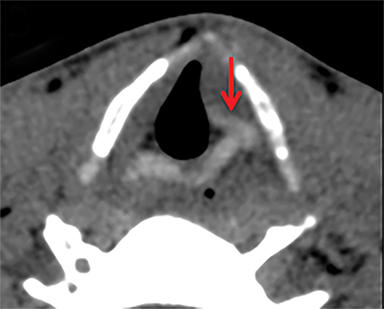
Cricoarytenoid subluxation or dislocation is more likely to occur during internal trauma such as intubation injury rather than blunt external laryngeal trauma. If the vocal fold is abnormally positioned in the setting of external trauma, recurrent laryngeal nerve (RLN) injury should be strongly considered.19 CT findings in RLN injury (Figure7) are that of enlargement of the ipsilateral laryngeal ventricle and piriform sinus, thickening and medial rotation of the aryepiglottic fold, anteromedial displacement of the arytenoid and medial displacement of the posterior vocal fold.20 This should be distinguished from cricoarytenoid joint luxations, which are characterized by displacement (anterior, medial, posterior, etc.) of the arytenoid cartilage, often with accompanying rotation or tilting of the cartilage with respect to the cricoid.15,21
Cricoarytenoid dislocations and subluxations are managed with operative reduction to create a pseudoarthrosis, with or without adjunctive medialization procedures such as vocal fold injections and/or thyroplasty. The prognosis for normal phonation is variable.2,11,22 In contrast, unilateral RLN injuries are often treated with medialization procedures if conservative management outcomes are suboptimal. There is of course no indication to attempt cricoarytenoid joint reduction if the injury is neurogenic.
Laryngotracheal rupture and separation
Frank laryngotracheal rupture or laryngotracheal separation is often accompanied by copious soft tissue gas, dissecting through fat planes in the neck and upper mediastinum. Laryngotracheal separation often occurs at the cricotracheal junction, as the cricoid is relatively immobile in the neck, but cricothyroid separation injuries are also possible. Signs of laryngotracheal separation include frank discontinuity of the airway, a widened cricotracheal interval with retraction of the trachea towards the mediastinum, as well as rupture of the cricothyroid membrane with cricothyroid malalignment or distraction. An abnormal axis of rotation between the cricoid and thyroid cartilages should raise suspicion for separation injury with cricothyroid membrane disruption.15 It is important to recognize that up to 50% of cricoid cartilage fractures are associated with laryngotracheal separation.15 Not surprisingly, there is also a high incidence of RLN injury with laryngotracheal separation. Rupture and separation are usually surgically repaired, although minor (<2cm) tracheal lacerations can be managed expectantly.16
Late sequela of laryngeal trauma
Untreated laryngeal cartilage fractures can lead to granulomatous remodeling with callus formation and deformation of the laryngeal skeleton, leading to dysphonia. Laryngeal callus can also be mistaken for tumor endoscopically.15 Untreated cricoarytenoid injuries can lead to ankylosis or malpositioned pseudoarthroses. Subglottic stenosis can be a complication of internal laryngotracheal injury and is usually from traumatic intubation, but up to 5% of cases are the consequence of external laryngeal trauma.15
Pharynx and esophagus
Anatomy
Anatomically, the pharynx is divided into three subsections, the most inferior of which (the hypopharynx) extends from the level of the hyoid bone to the inferior margin of the cricoid cartilage. The pharyngoesophageal junction is in the inferior hypopharynx and is also known as the cricopharyngeal (or upper esophageal) sphincter, the point at which the digestive tract is most narrow in the neck. It is also the level of Killian’s dehiscence, a point of anatomic weakness in the digestive tract between the inferior pharyngeal constrictor superiorly and the cricopharyngeus muscle inferiorly, where the pharyngeal wall is composed of only mucosa and serosa without intervening muscle. Consequently, this location is more frequently perforated with instrumentation and blunt trauma.23
Imaging evaluation
For the sake of simplicity, pharyngeal and esophageal trauma can be categorized as that resulting from blunt or penetrating external trauma or from internal trauma such as instrumentation or foreign body ingestion. The modern paradigm for imaging in penetrating neck trauma favors MDCTA if there are no hard signs warranting immediate neck exploration. In blunt neck trauma, patients will often get imaged with MDCTA in order to screen for cerebrovascular injury, providing opportunity to evaluate for pharyngoesophageal perforation. In foreign body ingestion, frontal and lateral neck radiographs are often the first line evaluation, but CT is more sensitive and specific, provides more information about precise location and can assist in identifying perforation, fistulas and abscesses.8 In particular for bone ingestions, some referring physicians may favor initial evaluation with CT.24 Sharp ingested foreign bodies such as fish and chicken bones have a predilection for lodging at the base of tongue/vallecula, at the piriform sinuses or in the postcricoid hyopharynx just above the narrow cricopharyngeal sphincter.8 They are also the foreign bodies most likely to result in perforation.
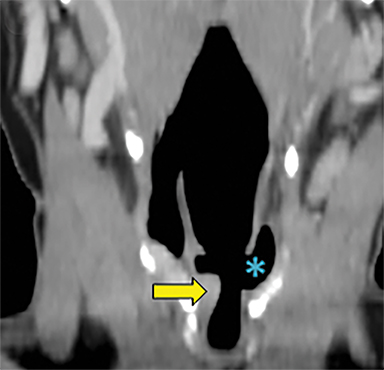
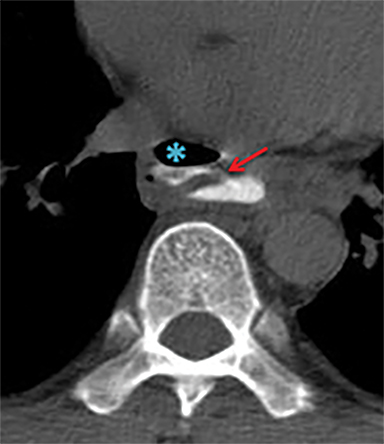
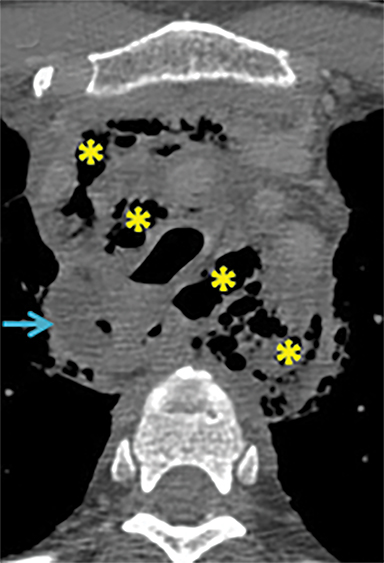
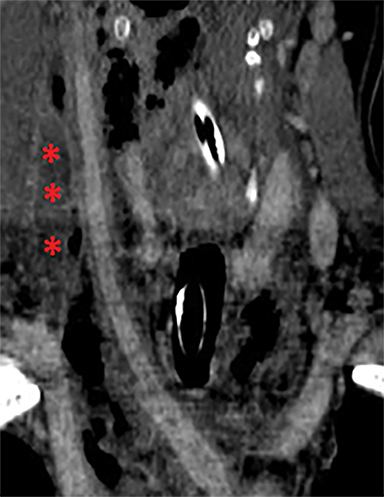
Signs of pharyngoesophageal perforation at CT include parapharyngeal or paraesophageal gas or fat stranding and occasionally frank communication of the esophageal or pharyngeal lumen with adjacent extraluminal collections of gas and/or fluid. If CT findings are inconclusive or if there is high clinical suspicion, particularly in penetrating trauma where the tract is in close proximity to the alimentary structures, further evaluation with CT or fluoroscopic esophagography may be warranted. Water-soluble contrast (Gastrografin) should be used first line, and can be followed with dilute barium. In Figure 8A, there is a gas and Gastrografin fluid collection in the mediastinum. Both fluoroscopic and CT esophagography have similar sensitivities for esophageal perforation, but rigid esophagoscopy detects small lacerations below the resolution of imaging, 11 although at the expense of requiring general anesthesia.
Management considerations
Management of pharyngoesophageal perforation depends on the location and size of the laceration. Some authors advocate conservative, expectant management of perforations < 2 cm if the risk of superinfection is considered low, such as with blunt trauma.23 Larger perforations carrying greater risk of infection undergo open primary closure with drainage of associated abscesses/collections. If the diagnosis of perforation is delayed >24 hours, morbidity increases. Mortality of patients with a missed diagnosis of pharyngoesophageal perforation approaches 20%.7 Complications are severe, and include mediastinitis, abscess and sepsis (Figures 8B and C) Of note, patients undergoing operative repair of airway trauma will uniformly undergo screening rigid esophagoscopy to exclude subtle concurrent esophageal perforation.11 In regards to management of ingested foreign bodies, up to 10-20% will require removal endoscopically. Only approximately 1% require surgical removal.8
Conclusion
Although rare, blunt and penetrating trauma to the soft tissue structures of the neck is associated with high morbidity and mortality. CT is increasingly utilized to simultaneously evaluate the vascular anatomy and the upper aerodigestive structures. While management of laryngotracheal traumatic injury continues to evolve, knowledge of current practices allows radiologists to assist in triage algorithms and help guide surgical and interventional treatments.
References
- Gussack GS, Jurkovich GJ, Luterman A. Laryngotracheal trauma: A protocol approach to a rare injury. Laryngoscope. 1986;96(6): 660-665.
- Atkins BZ, Abbate S, Fisher SR, et al. Current management of laryngotracheal trauma: Case report and literature review.J Trauma. 2004;56(1):185-190.
- Demetriades D, Velmahos GG, Asensio JA. Cervical pharyngoesophageal and laryngotracheal injuries.World J Surg. 2001;25(8): 1044-1048.
- Steenburg SD, Sliker CW, Shanmuganathan K, et al. Imaging evaluation of penetrating neck injuries.RadioGraphics. 2010;30(4): 869-886.
- Biffl WL, Moore EE, Offner PJ, et al. Blunt carotid arterial injuries: Implications of a new grading scale.J Trauma. 1999;47(5):845-853.
- Bromberg WJ, Collier BC, Diebel LN, et al. Blunt cerebrovascular injury practice management guidelines: The Eastern Association for the Surgery of Trauma.J Trauma. 2010;68(2): 471-477.
- Sung EK, Nadgir RN, Sakai O. Computed tomographic imaging in head and neck trauma: What the radiologist needs to know.Semin Roentgenol. 2012;47(4): 320-329.
- Pinto A, Muzj C, Gagliardi N, et al. Role of imaging in the assessment of impacted foreign bodies in the hypopharynx and cervical esophagus.Semin Ultrasound CT MR. 2012;33(5): 463-470.
- Mendels EJ, Brunings JW, Hamaekers AE, et al. Adverse laryngeal effects following short-term general anesthesia: A systematic review.Arch Otolaryngol Head Neck Surg.2012;138(3): 257-264.
- Bell RB, Osborn T, Dierks EJ, et al. Management of penetrating neck injuries: A new paradigm for civilian trauma.J Oral Maxillofac Surg. 2007;65(4):691-705.
- Schaefer SD. Management of acute blunt and penetrating external laryngeal trauma. Laryngoscope.2014;124(1): 233-244.
- Apffelstaedt JP, Muller R. Results of mandatory exploration for penetrating neck trauma.World J Surgery. 1994;18(6):917-919; discussion 920.
- Liang T, Tso DK, Chiu RY, et al. Imaging of blunt vascular neck injuries: A review of screening and imaging modalities.AJR Am J Roentgenol. 2013;201(4): 884-892.
- Liang T, Tso DK, Chiu RY, et al. Imaging of blunt vascular neck injuries: A clinical perspective. AJR Am J Roentgenol. 2013;201(4): 893-901.
- Becker M, Leuchter I, Platon A, et al. Imaging of laryngeal trauma. Eur J Radiol. 2014;83(1): 142-154.
- Prokakis C, Koletsis EN, Dedeilias P, et al. Airway trauma: A review on epidemiology, mechanisms of injury, diagnosis and treatment.J Cardiothorac Surg. 2014;9: 117-8090-9-117.
- Schaefer SD. The acute management of external laryngeal trauma. A 27-year experience.Arch Otolaryngol Head Neck Surg. 1992;118(6): 598-604.
- Duda JJ, Lewin JS, Eliachar, I. MR evaluation of epiglottic disruption.AJNR Am J Neuroradiol. 1996;17(3): 563-566.
- Schroeder U, Motzko M, Wittekindt C, et al. Hoarseness after laryngeal blunt trauma: A differential diagnosis between an injury to the external branch of the superior laryngeal nerve and an arytenoid subluxation. A case report and literature review.Eur Arch Otorhinolaryngol. 2003; 260(6): 304-307.
- Paquette CM, Manos DC, Psooy BJ. Unilateral vocal cord paralysis: A review of CT findings, mediastinal causes, and the course of the recurrent laryngeal nerves.RadioGraphics. 2012;32(3): 721-740.
- Hiramatsu H, Tokashik R, Kitamura M, et al. New approach to diagnose arytenoid dislocation and subluxation using three-dimensional computed tomography.Eur Arch Otorhinolaryngol. 2010; 267(12): 1893-1903.
- Sataloff, RT. Atlas of Endoscopic Laryngeal Surgery. New Delhi: Jaypee Brothers Medical Publishers; 2011.
- Cross KJ, Koomalsingh KJ, Fahey TJ, et al. Hypopharyngeal rupture secondary to blunt trauma: Presentation, evaluation, and management. J Trauma. 2007;62(1): 243-246.
- Eliashar E, Dano I, Dangoor E, et al. Computed tomography diagnosis of esophageal bone impaction: A prospective study. Ann Otol Rhinol Laryngol. 1999;108(7 Pt 1): 708-710.
Citation
AC M, A U. Imaging blunt and penetrating trauma to the neck: Clinical relevance and management. Appl Radiol. 2016;(7):14-19.
July 2, 2016