Epiploic appendagitis

Epiploic appendagitis
Findings
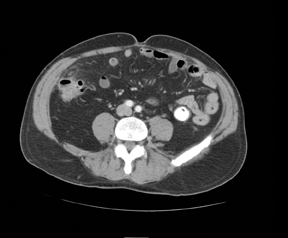
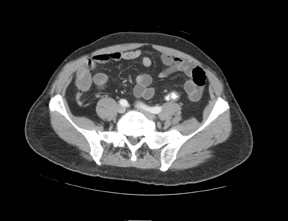
Three noncontiguous, contrast-enhanced axial computed tomography (CT) images of the abdomen revealed a 2- x 1-cm fat-attenuated,ovoid mass anterior to the cecum with a hyperdense center and adjacent inflammatory stranding (Figures 1 and 2). The appendix was normal (Figure 3).
Discussion
Epiploic appendagitis, a relatively rare entity, has been diagnosed with increasing frequency during the era of multislice CT. Acute epiploic appendagitis may clinically mimic acute diverticulitis or acute appendicitis, as patients frequently present with acute onset, lower-quadrant pain though they are commonly afebrile and without leukocytosis.1
The most common etiologies of this entity are venous thrombosis (secondary) or torsion or incarceration of an epiploic appendage within ahernia sac (primary). The common pathway is venous outflow obstruction, leading to engorgement and inflammation of the epiploic appendage. The most common sites of involvement are the sigmoid colon, the descending colon, and the ascending colon (in order of decreasing frequency). Characteristic CT features include an ovoid, fat-density lesion measuring <5cm, typically along the anterior aspect of the colon with adjacent inflammatory changes.2,3 Central hyperdensity is related to venous congestion. Thickening of the visceral peritoneum may also be seen,although it tends to be associated with omental infarct.2
Important clinical and radiologic mimics of acute epiploic appendagitis include acute appendicitis, acute diverticulitis, and omental infarct.2,4 Lack of laboratory abnormalities help in eliminating acute appendicitis. The imaging appearance is also significantly different, with a tubular soft-tissue density surrounded by mesenteric stranding and, possibly, free fluid seen in appendicitis. Acute diverticulitis typically demonstrates significant bowel wall thickening and extraluminal free air, which are absent with epiploic appendagitis.1 These patients also commonly have fever and leukocytosis. Epiploic appendages may become secondarily inflamed, complicating the diagnosis. Omental infarct presents with a heterogenous soft tissue density >5 cm and without the circumscribed, hyperattenuating ring of epiploic appendagitis.4,5 The location may also differ, as omental infarct is typically located anterior to the ascending or transverse colon while epiploic appendagitis is most often found in the sigmoid region.1,5
Conclusion
By recognizing typical imaging features of epiploic appendagitis, the radiologist plays a central role in preventing needless surgery and facilitating appropriate, conservative management.
- Singh, AK, Gervais DA, Hahn PF, et al. Acute epiploic appendagitis and its mimics. Radiographics. 2005;25:1521–1534.
- Legome EL, Belton AL, Murray RE, et al. Epiploic appendagitis: The emergency department presentation. J Emerg Med. 2002;22:9–13.
- Sirvanci M, Tekelioglu MH, Duran C, et al. Primary epiploic appendagitis: CT manifestations. Clin Imaging. 2000;24:357–361.
- van Breda Vriesman AC, Puylaert JB. Epiploic appendagitis and omental infarction: Pitfalls and look-alikes. Abdom Imaging. 2002;27:20–28.
- Rioux M, Langis P. Primary epiploic appendagitis: Clinical, US, and CT findings in 14 cases. Radiology. 1994;191:523–526.
