Emphysematous pyelonephritis


CASE SUMMARY
A 74-year-old obese woman with a long-standing history of uncontrolled type II diabetes mellitus was admitted to the hospital for an acute asthma exacerbation. She developed severe abdominal pain on the 6th day of admission. The abdomen was tender to palpation in the right lower quadrant, right costovertebral angle tenderness was present, bowel sounds were present and there was no rebound tenderness. Later in the day the patient developed a fever, hypotension, tachycardia and leukocytosis. She was noted to be hyperglycemic for several days. She was sent to our department for a CT scan of the abdomen and pelvis.
IMAGING FINDINGS
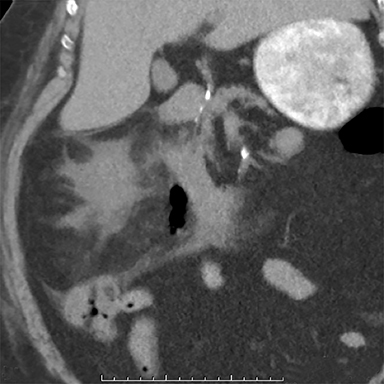
A CT scan of the abdomen and pelvis performed without IV contrast, due to the patient’s allergy to contrast, showed gas within the right renal parenchyma, collecting system, ureter and perinephric space. There was also infiltration of and fluid in the right perinephric fat and mild right hydronephrosis. No fistula was seen between the gastrointestinal and genitourinary tracts.
DIAGNOSIS
Emphysematous pyelonephritis
DISCUSSION
Emphysematous pyelonephritis (EPN) is a radiologically diagnosed life-threatening, necrotizing infection of the kidneys characterized by the presence of gas in the renal parenchyma and its surrounding tissue.1 Likely due to the higher incidence of urinary tract infections, EPN is seen more commonly in females. The greatest risk factor for developing EPN is uncontrolled diabetes mellitus. In nondiabetic patients, anatomic anomalies such as urinary tract obstructions or urinary calculi, or an immunocompromised state can be the predisposing factor.2
EPN is caused by glucose-fermenting bacteria; the most common causative organism being Escherichia coli, followed by Klebsiella pneumonia, and Proteus mirabilis.3,4 Although the exact pathogenesis of EPN is unclear, it has been suggested that high levels of glucose along with impaired vascular blood supply allows for an ideal environment for gram-negative anaerobic bacteria to produce gas by fermenting lactate and glucose. It is important to note that nondiabetic patients also get EPN; thus, this theory does not fully explain the pathogenesis.1
Clinically, most patients present symptomatically with fever and abdominal, flank or back pain consistent with signs of pyelonephritis and with laboratory studies that show leukocytosis and occasionally thrombocytopenia.3-5 The diagnosis of EPN is difficult based on history, physical exam and laboratory values alone; thus, radiological imaging is necessary to confirm the diagnosis.
Plain X-ray of the abdomen may show abnormal formations of gas. However, plain radiography is not the diagnostic method of choice. Ultrasound may also show an abnormal kidney with nondependent echoes, but there may be misdiagnoses due to the presence of adjacent bowel gas or calculi, which may cause confusion. Although plain radiography and ultrasound may suggest EPN, computed tomography (CT) of the abdomen is more sensitive, allows for more accurate staging of the disease and is considered the gold standard for diagnosis.6
Several classification methods for EPN exist for both plain radiograph and CT. One of the early classification systems was introduced by Michaeli et al; the plain radiograph and intravenous pyelogram were used to categorize EPN into three stages: Stage I describes gas in the renal parenchyma or perinephric tissue; stage II describes gas in the kidney and its surroundings; and stage III indicates extension of gas through fascia or bilateral disease.1 Wan et al classify EPN based on CT scanning into two different types: Type I shows either renal necrosis with presence of gas but no fluid, or streaky mottled gas patterns, indicating a worse prognosis. Type II, meanwhile, is defined by parenchymal gas associated with fluid in the renal parenchyma, perinephric space or collecting system and the absence of streaky or mottled gas pattern. It has a more favorable prognosis than Type I.4
The classification of EPN has evolved over time and has become increasingly more comprehensive. The more detailed CT classification by Huang and Tseng correlates with the management of various stages of EPN. Huang and Tseng’s classification has four different classes. Class 1 indicates gas in the collecting system only. Patients with Class 1 EPN have the best prognosis and can be managed medically with parenteral antibiotics and fluid, electrolytes and glucose control. Class 2 represents gas in the renal parenchyma; management of patients in this class consists of antibiotics plus percutaneous catheter drainage (PCD) and if present, relief of any obstruction in the urinary tract. Class 3 is divided into two sub-categories, A and B. Class 3A describes gas or abscess to perinephric space and Class 3B describes gas or abscess extending beyond the kidney. Management of class 3 EPN depends on the patient’s risk factors, which include thrombocytopenia, acute renal failure, disturbance of consciousness and shock. If patients have no or one risk factor, they can initially be managed medically with antibiotics and PCD. If patients have 2 or more risk factors, nephrectomy is indicated and will help the prognosis. Class 4 indicates either bilateral or solitary kidney involvement; class 4 management of bilateral renal involvement calls for bilateral PCD with medical antibiotics. If that fails, nephrectomy is indicated. Class 4 management of patients with a solitary kidney also initially calls for PCD with antibiotics, with nephrectomy indicated on failure of that treatment.5
Our patient with a longstanding history of poorly controlled diabetes mellitus suffered an acute episode of EPN complicated by septic shock and renal failure during her hospitalization for an acute asthma exacerbation. She was treated conservatively with antibiotics for the pyelonephritis and with a ureteral stent to relieve the hydronephrosis resulting from her unstable critical condition. Although nephrectomy is considered the most efficient treatment for EPN, many patients become too unstable for invasive procedures. Thus, conservative methods with medical management and minimally invasive procedures should be aggressively pursued. Our patient recovered with only conservative medical management.
CONCLUSION
Emphysematous pyelonephritis is a potentially serious fulminant bacterial infection of the kidneys characterized by gas in the collecting system, renal parenchyma and perinephric tissues. Prompt diagnosis of EPN is imperative and should be followed by aggressive medical management with antibiotics to minimize life-threatening complications and the potential need for more invasive intervention.
REFERENCES
- Michaeli J, Mogle P, Perlberg S, Heiman S, Caine M. Emphysematous pyelonephritis. J Urol. 1984; 131:203-208.
- Ubee SS, McGlynn L, Fordham M. Emphysematous pyelonephritis. Br J Urol Int. 2010;107: 1474-1478.
- Kuo CY, Chen TC, Lin WR, et al. Clinical features and prognostic factors of emphysematous urinary tract infection. J Microbiol Immunol Infect. 2009; 42:393-400.
- Wan YL, Lee TY, Bullard M, Tsai CC. Acute gas-producing bacterial renal infection: Correlation between imaging findings and clinical outcome. Radiology. 1996; 198:433-438.
- Huang JJ, Tseng CC. Emphysematous pyelonephritis: Clinicoradiological classification, management, prognosis, and pathogenesis. Arch Intern Med. 2000;160:797-805.
- Craig WD, Wagner BJ, Travis MT. Pyelonephritis: Radiologic-pathologic Review. Radiographics. 2008; 28:255-276.
