Breast-Specific Gamma Imaging
Images


In the diagnosis of breast cancer, anatomic findings on mammography and ultrasound imaging can sometimes be inconclusive, particularly in women with dense breast tissue and those who have natural changes within the breast parenchyma. Functional imaging, such as Breast-Specific Gamma Imaging (BSGI) with the Dilon 6800 gamma camera (Figure 1), can often overcome these limitations and provide crucial information that cannot be found with anatomic imaging.
"In cellular biology, the first thing to change with cancer is the function, not the gross anatomy," explained Ted Fogarty, MD, Staff Radiologist at Medcenter One Hospital, Bismarck, ND, and Chairman of Radiology, University of North Dakota School of Medicine, and a shareholder in Dilon Technologies. "Mammography just looks at the anatomy," said Milton J. Guiberteau, MD, FACR, Chief, Nuclear Radiology in the Department of Medical Imaging, and Director of the Women's Care Mammography Clinic at CHRISTUS St. Joseph Hospital, Houston, TX. "BSGI, on the other hand, reveals the function of the tissue, enabling clinicians to more clearly determine if the anatomic changes are benign or are suspicious for malignancy."
The Dilon 6800: Advanced Technology Significantly Improves Clinical Results
Functional imaging of the breast is not a new concept. It was first attempted many years ago using a standard gamma camera; however, the limitations inherent in the older equipment did not allow for the reliable detection of many cancers, such as sub-centimeter lesions and DCIS (Ductal Carcinoma In Situ). Furthermore, the standard gamma cameras were unable to replicate mammographic views, which made correlation between the functional and anatomic data difficult.
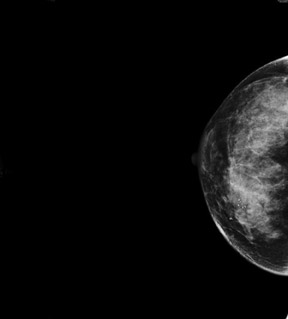
Unlike other gamma cameras, the Dilon 6800 has been optimized for breast imaging and is capable of detecting lesions as small as 3 mm. Its sensitivity has been found to be similar to mammography at approximately 96%, but its specificity is significantly higher at 92%, and its negative predictive value has been shown to be as high as 99%. In addition, BSGI with the Dilon 6800 replicates the patient positioning used in mammography (Figure 2), thereby providing an easily correlated functional map to the structural abnormality.
BSGI in Clinical Practice
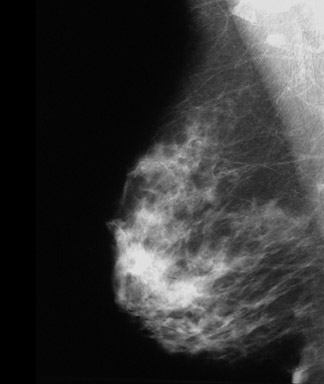
BSGI is most commonly used for those patients who have equivocal mammography or ultrasound findings. "Mammography is very good at detecting cancer in women who have easy-to-read mammogram patterns, but it's not so good for women who have dense patterns," said Fogarty, explaining that mammograms of heterogeneously dense and very dense breasts often are very nonspecific. With BSGI, the diagnostic quality of the image is not affected by tissue density or other structural changes, such as scars or implants. "The sensitivity is the same in both fatty breast and dense breasts," said Guiberteau. "We use BSGI on patients with dense breasts who have findings that are not elucidated by diagnostic mammography," he continued, "and in patients who have implants or postsurgical, post-chemotherapy, or postradiation lesions."
A plus to its utility in initial diagnosis is that BSGI is also helpful in detecting additional, unsuspected lesions in women with a known carcinoma. "In patients with a known cancer diagnosis, we use BSGI to help determine the extent of involvement in that breast and to gather information about the other breast," said Tricia A. Kelly, MD, Assistant Professor of Surgery and Associate Director of the Breast Care Center at George Washington University, Washington, DC. "In many cancer patients, we have seen additional foci in the involved breast and we've picked up foci in the opposite breast."
Such BSGI findings can alter surgical planning and follow-up regimens. "If we find a second, remote carcinoma, that patient may no longer be a candidate for breast conservation surgery and might need a mastectomy," said Kelly.
BSGI may also be used to help clarify lymph node status. "For example, in a patient with a known cancer diagnosis without any clinically significant lymph node findings, we may see uptake in the axilla on the BSGI," explained Kelly. "If we see what looks like lymph node involvement on BSGI, we may alter what we recommend as far as a sentinel node biopsy versus axillary dissection."
Integrating BSGI in the Breast Center
The compact, mobile design of the Dilon 6800 allows the system to be integrated into the breast center, facilitating a smooth continuum of care and allowing for rapid results for patients' peace of mind. In fact, in many facilities, patients can proceed directly from diagnostic mammography to BSGI during the same visit.
For the patient, the BSGI is nearly identical to the familiar mammogram, but without the uncomfortable compression. Once the examination is completed, patients can often get their results right away. "We always compare our BSGI study with the patient's mammogram, ultrasound, magnetic resonance imaging studies, history, and anything else that is available," noted Guiberteau, "but if the patients are willing to wait a few minutes, we are usually able to give them their results right away."
Learning Curve
"As for the learning curve, like any exam, the technologist must be adequately trained to get the proper images, but it can be readily learned," said Guiberteau. "For physicians reading the study, I would not say the learning curve is steep, but you have to be able to distinguish between a focus that looks significant as opposed to a focus that looks like the background of normal breast tissue. With the Dilon camera, the interpretation is not difficult."
"The other learning curve issue is learning to trust the technology," added Fogarty, "because you are so trained to use structurally suspicious findings to determine how to proceed. Early on, we did some biopsies on things that had shown up as shadowing areas on ultrasound or consistent masses under compression, but the findings on BSGI were negative, so we began to trust the technique more."
Case Report
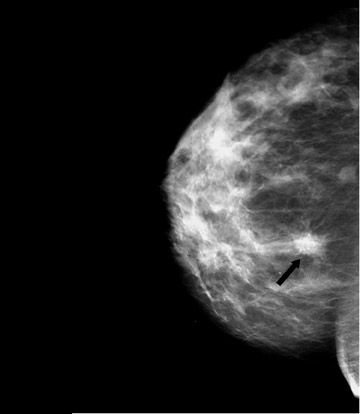
An 82-year-old woman with moderate bilateral stable dense breast parenchyma presented with a new nodular density that was noted on mammography (Figure 3). The findings were classified as BIRADS 4, with no cysts or solid masses noted on the ultrasound examination.
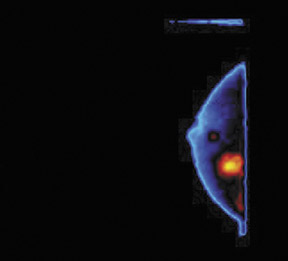
The patient underwent BSGI, which showed two foci of significant uptake (Figure 4). One was consistent with the nodular density noted in the mammogram and the other was within the area of stable dense breast tissue. The histopathology findings for this patient indicated infiltrating ductal carcinoma in both sites. In this case, BSGI detected a second site of carcinoma that had not previously been located with other modalities, thereby changing the course of treatment for this patient.
Conclusion
"This is one of those cases in medicine in which not only is it a great piece of technology, it's actually a money-saving use of resources," concluded Fogarty. "When we find a 1-cm cancer with BSGI on a woman who has a total white-out on a mammogram and we are able to catch it as stage 1 disease, we end up saving the healthcare system hundreds of thousands of dollars and we save that woman's life."
Contact Information
Dilon Technologies LLC
12050 Jefferson Ave, Newport News, VA 23606
877.GO DILON info@dilon.com
www.dilon.com