Mammographic and ultrasound evaluation in patients with implantable breast mesh
By M Rizer, R Alexander, SS Kaplan
CASE SUMMARY
We present a 36-year-old female who was seen for initial voluntary screening mammography with a history of breast mesh placement immediately following a voluntary breast reduction surgery at the age of 18 in 1986. As per the patient, the breast mesh was placed according to the Ricardo A. Bustos Technique (Mammary Prosthesis, Patent # US 4840629). There was no palpable abnormality on physical exam.
IMAGING FINDINGS
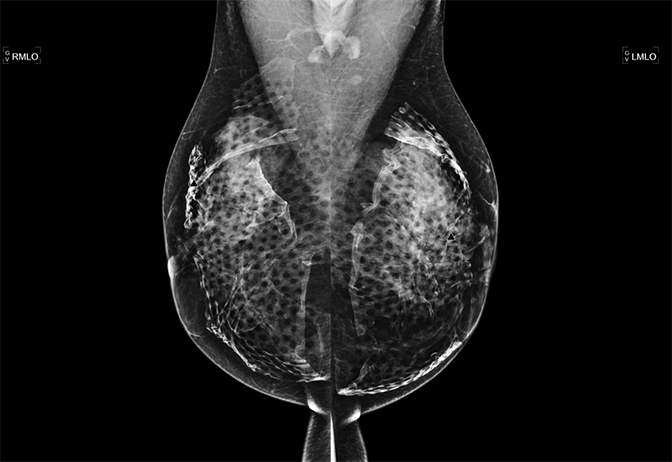
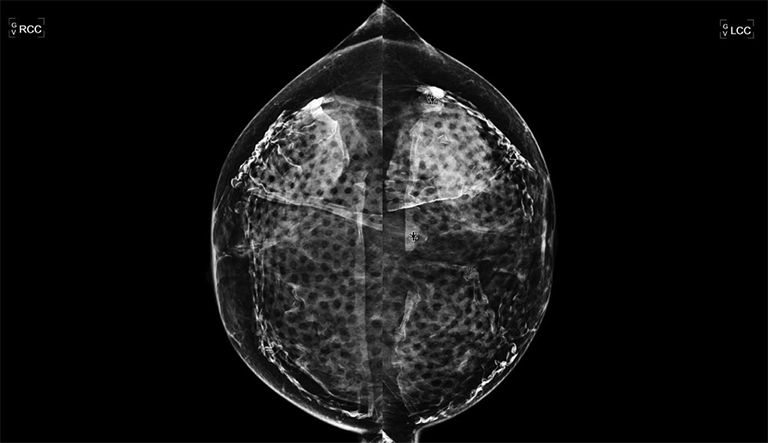
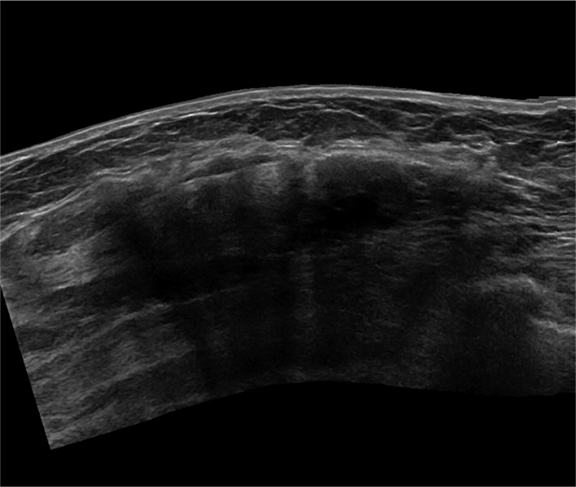
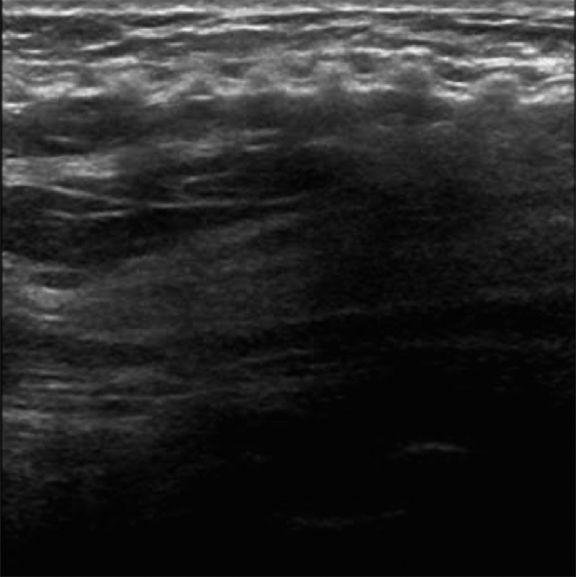
Mammographic evaluation was severely limited by the implanted mesh bilaterally on both craniocaudal (CC) and mediolateral oblique (MLO) views. Further evaluation was recommended with ultrasound. Unfortunately, this too was limited due to severe posterior acoustic shadowing from the mesh material (Figures 1-4).
DISCUSSION
The variety of techniques available for breast reconstruction is almost as diverse as breast pathology. The most common procedures include augmentation mammoplasty and mammopexy. According to the American Society of Plastic Surgeons, approximately 286,274 breast augmentations and 89,067 were performed in 2012, making it the top cosmetic surgery procedure among women.1 Despite advanced techniques, recurrent ptosis of the breasts or displacement of the breast implants is common, due to the inherent weakness of the tissues. Breast reconstruction following mastectomy also continues to remain a topic of interest in plastic surgery and oncology in an effort to preserve aesthetics and decrease the potential psychological distress related to mastectomy.
Over the past several years, there has been a paradigm shift in the traditional options and techniques available for breast reconstruction owing to innovations and advancements. As a result, the number of women choosing breast reconstruction has increased not only because of the expanded options, but also because surgical outcomes have improved.2 Breast surgeons are now able to safely and effectively perform skin-sparing and occasionally nipple-areola-sparing mastectomy to preserve the natural skin envelope of the breast, which remains weak without the underlying ligamentous support.
The use of surgical mesh implants has become a topic of discussion in recent years with multiple different mesh materials being used for reinforcement since the 1980s. Though few materials are approved for use in the United States, many more are approved abroad. In the past, the variety of implantable breast mesh materials had not been fully evaluated with respect to their effect on mammography evaluation or long-term biological effects. This continues to be a concern, as the long-term implications of mesh use in breast surgery remain unclear. Further studies need to be performed on the variety of mesh materials available for breast reconstruction and their implications on radiological breast evaluation.
CONCLUSION
We recommend that women who have implantable surgical mesh in the breast for breast reduction establish a baseline with mammographic and ultrasound evaluation. This is particularly important in patients who undergo mastectomy for breast cancer, as monitoring may be degraded, and recurrent lesions have the potential of being missed. Patients who do not have a baseline and an obscuring breast mesh on mammography may benefit from tomosynthesis or MR evaluation.
REFERENCES
- American Society of Plastic Surgeons. 2012 Plastic Surgery Statistics Report. http://www.plasticsurgery.org/Documents/news-resources/statistics/2012-Plastic-Surgery-Statistics/full-plastic-surgery-statistics-report.pdf
- Nahabedian MY. Acellular dermal matrices in primary breast reconstruction: Principles, concepts, and indications. Plast Reconstr Surg. 2012;130;44S.
