Diffuse atypical papillomatosis of the breast
CASE SUMMARY
A 50-year-old woman presented with a lump in the right breast at baseline mammographic evaluation. The patient denied any associated symptoms. Her background revealed no significant family history or personal history of breast cancer.
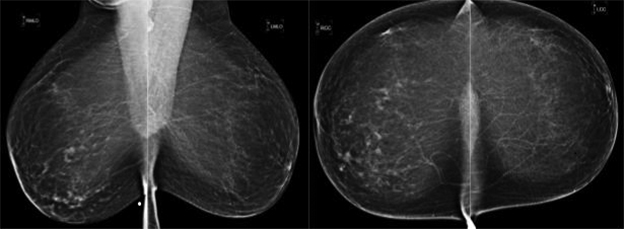
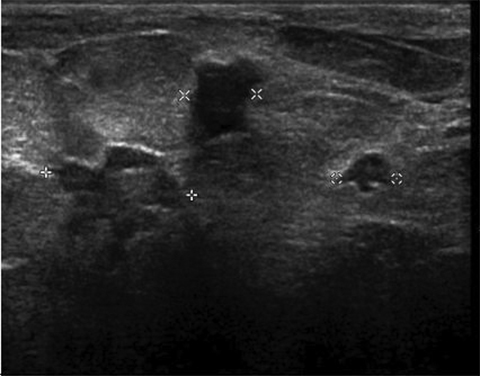
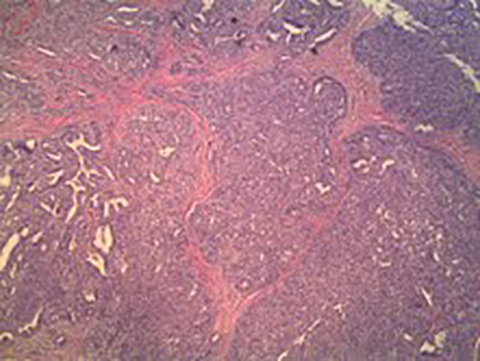
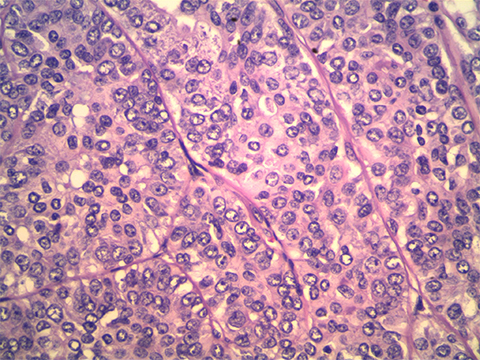
IMAGING FINDINGS
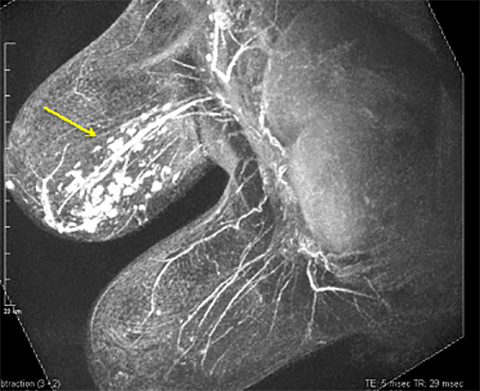
A diagnostic digital mammogram revealed multiple focal, small, mass-like asymmetries in the right breast (Figure 1). Targeted ultrasound confirmed the presence of multiple lobulated and irregular solid hypoechoic vascular sub-centimeter masses that correlated with the mammographic and palpable findings (Figure 2). One lesion was selected for biopsy, yielding a diagnosis of atypical papilloma. Surgical excision was recommended due to the suggested extent of disease and presence of atypia (Figure 3A and 3B).
Preoperative MRI (Figure 4) confirmed and better defined the presence of multiple right breast enhancing masses arranged in a segmental distribution, extending anterior to posterior depth and encompassing the 3 o’clock to 7 o’clock positions. The left breast was unremarkable. Two additional right-breast lesions depicted by MRI were isolated for targeting under ultrasound and then biopsied, again demonstrating atypical papillomas.
With multicentric atypical papillomas spanning a large area of the right breast, local excision or lumpectomy had the potential of leaving behind disease and would have certainly resulted in suboptimal cosmetic outcome. Therefore, the patient and surgeon agreed to a right total mastectomy, which would ensure removal of all evidence of disease, in addition to reducing the patient’s risk of future breast cancer in the right breast. Due to the patient’s heightened anxiety and fear, the decision was made to also perform a prophylactic left total mastectomy. The patient was offered breast reconstruction, but she refused this option. Bilateral total mastectomy confirmed extensive right breast intraductal papillomatosis with cytologic atypia centered in the inferomedial right breast measuring 6 cm × 5 cm × 4.5 cm. One small intraductal papilloma was evident on the left in the mastectomy specimen that was occult to imaging and clinical workup. There was no pathologic evidence of invasive carcinoma in either breast.
DIAGNOSIS
Diffuse atypical papillomatosis of the breast
DISCUSSION
Papillary breast lesions encompass a spectrum of masses, which pathologically demonstrate fronds attached to the inner mammary duct wall by a fibrovascular core with both epithelial and myoepithelial cells.1-3 Although not frankly malignant, papillary disease is associated with an increased risk of invasive breast cancer.2 The epithelial component of papillary lesions can vary, resulting in metaplasia, hyperplasia, atypical intraductal hyperplasia, or carcinoma in-situ.3 Histologically, distinguishing between the benign, borderline, or malignant types can be difficult.1,4 Papillary pathology encompasses isolated intraductal papillomas, papillomatosis with or without atypia, and papillary adenocarcinoma with or without invasion.4-5
The location and number of papillary lesions can be solitary and central (subareolar) or multifocal and peripheral involving the terminal lobular units. Detection of disease within the mammary duct system can be difficult, and the clinical presentation and risk of malignancy for the patient differs between these two groups.4
Solitary papillomas occur more commonly in women between 30 to 50 years of age, often complaining of spontaneous serous or serosanguinous nipple discharge. This type of papillary disease is associated with only a slightly increased risk of breast carcinoma (1.5 to 2.0 times).1,3 Papillomas may demonstrate a spectrum of atypical features that include atypical ductal hyperplasia (ADH) or low-grade DCIS. Papillary carcinoma is very uncommon and represents only 2% of all breast cancers.2 There is no consensus on the histologic criteria for diagnosing atypia in papillomas. Some pathologists suggest atypia when papillomas demonstrate epithelial proliferation of 3 mm or greater in size, while others assign the diagnosis when the atypical proliferation exhibits features similar to low- grade DCIS.4
Multiple papillomatosis is estimated to occur in approximately 10% of papillary cases. “Multiple” has been traditionally defined as five or more separate papillomas within a segment of breast tissue.1,4 Multiple papillomatosis is commonly bilateral. The true size of a papilloma may be larger than it appears by clinical or radiologic evaluation, resulting in the potential for incomplete excision and subsequent recurrence.4 Tissue sampling from core biopsy may not adequately represent the entire lesion5; foci of ADH or DCIS elsewhere in a papilloma may be missed at percutaneous biopsy.5
Patients with papillomatosis are typically younger than those with solitary lesions, and are often asymptomatic. A subset of this form of papillary disease includes juvenile papillomatosis, where a young woman presents with a palpable abnormality, at first clinically thought to be a fibroadenoma. Pathologic evaluation, however, shows papillomatosis and widespread cyst formation. Importantly, juvenile papillary pathology is associated with a strong family history of breast cancer.6 Multiple papillomas may be highly susceptible to malignant transformation, likely due to their slightly different cytologic architecture, and are also associated with a higher risk (3.0) of hyperplasia, atypia, DCIS, sclerosis adenosis, and radial scar.1,4 Papillomatosis with atypia has a 7.0 higher relative risk of developing breast carcinoma.4
Mercado et al showed that papillary lesions surgically excised were upgraded to either ADH or DCIS in 26% of patients.5 The atypical component can involve a small component of a papilloma, and a study by Page et al revealed that 63% of cases showed ADH in the surrounding tissue upon surgical excision.5,7 Based on several studies, the histologic underestimate, or the number of lesions determined to be benign on biopsy but malignant upon excision, ranges from 30% to 67% for papillomas with atypia.2,8-9
The radiologic appearance of papillomatosis can be quite varied.1,10 Mammographically, papillomas can be oval, round, or lobulated well-circumscribed or spiculated masses. They may also appear as an asymmetric density or as a cluster of nodules, with or without calcification. Under ultrasound, they can be circumscribed round, oval, lobulated solid or complex masses.1
Papillomas may also demonstrate a variable appearance and enhancement features on MRI.1 MRI is highly sensitive in detecting papillomas and the extent of multicentric disease in papillomatosis.4,10 MRI provides excellent depiction of the position of lesions for targeted sonographic evaluation. Given the significant histologic underestimation of even asymptomatic papillomas at percutaneous biopsy, surgical excision (with a 10-mm clear margin) should be pursued.5
CONCLUSION
The breast surgeon and imager should be aware of the challenges in detecting, diagnosing, and managing papillary disease, which encompasses a wide spectrum of pathology and has varying levels of clinical significance. Surgical options may change with associated cytologic atypia and diffuse involvement, as these features are associated with a much higher risk of associated breast malignancy and upgrade at surgery. If the disease is extensive, mastectomy may provide the best surgical option. Further, women with breast papillomatosis have increased risk of bilateral breast disease, as our patient was found to have at (prophylactic) mastectomy. Patient education regarding the future risks of bilateral and recurrent disease is important so that a better-informed decision can be made for treatment.
REFERENCES
- Al Sarakbi W, Worku D, Escobar PF, Mokbel K. Breast papillomas: Current management with a focus on a new diagnostic and therapeutic modality. Int Semin Surg Oncol. 2006;3:1.
- Sydnor MK, Wilson JD, Hijaz TA, et al. Underestimation of the presence of breast carcinoma in papillary lesions initially diagnosed at core-needle biopsy. Radiology. 2007;242:58-62.
- Debnath D, Al-Okati D, Ismail W. Multiple papillomatosis of breast and patient’s choice of treatment. Patholog Res Int. 2010; 540-590.
- Ueng S, Mezzetti T, Tavassoli F. Papillary neoplasms of the breast: a review. Arch Pathol Lab Med. 2009;133: 893-907.
- Mercado CL, Hamele-Bena D, Oken SM, et al. Papillary lesions of the breast at percutaneous core-needle biopsy. Radiology.2006;238:801-808.
- Muttarak M, Lerttumnongtum P, Chaiwun B, Peh WCG. Spectrum of papillary lesions of the breast: Clinical imaging, and pathologic correlation. AJR Am J Roentgenol. 2008;191:700-707.
- Page DL, Salhany KE, Jensen RA, Dupont WD. Subsequent breast carcinoma risk after biopsy with atypia in a breast papilloma. Cancer. 1996;78:258-266.
- Liberman L, Bracero N, Vuolo MA, et al. Percutaneous large-core biopsy of papillary breast lesions. AJR Am J Roentgenol. 1999;172:331-337.
- Rosen EL, Bentley RC, Baker JA, Soo MS. Imaging-guided core needle biopsy of papillary lesions of the breast. AJR Am J Roentgenol. 2002;179:1185-1192.
- Son EJ, Kim EK, Kim JA, et al. Diagnostic value of 3D fast low-angle show dynamic MRI of breast papillomas. Yonsei Med J. 2009;50:838-844.
