A pictorial review of the anatomy and common pathology of the buccal space: “The overlooked space”
Images











Dr. Seelagan is a Musculoskeletal Fellow, Department of Diagnostic Radiology, and Dr. Noujaim is Chief of Head & Neck Radiology, Division of Neuroradiology, Department of Diagnostic Radiology, William Beaumont Hospital, Royal Oak, MI.
This paper was originally presented at the American Society of Neuroradiology 42nd Annual Meeting, Washington State Convention & Trade Center, Seattle, WA. June 5-11, 2004.
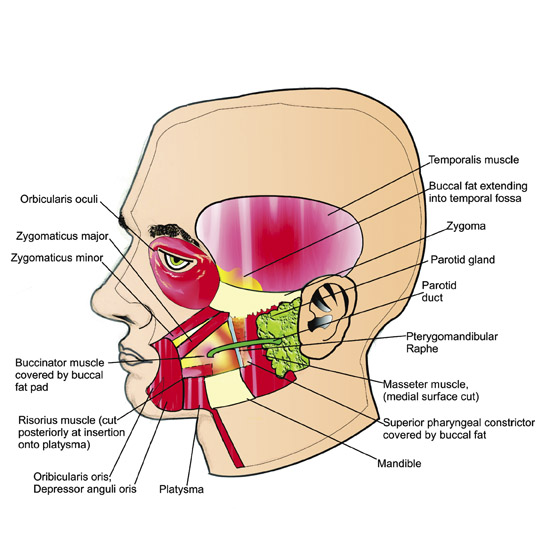
The head and neck region is divided by fascial planes into a series of compartments. Knowledge of these compartments and their contents limits the daunting gamut of head and neck pathology to a manageable differential diagnosis. The buccal space is one such compartment that has not received an equitable representation in the literature relative to other compartments, primarily because of the predominance of adipose tissue and its small size. However, because of the close relationship to important structures both in and around this space, a variety of pathology may be seen. A meta-analysis of the literature reveals the most common pathology of the buccal space to be salivary gland tumors, especially pleomorphic adenoma. 1 Other common etiologies of lesions are hemangiomas, 2 infection, and benign and malignant lymph nodes. Patients with buccal space masses usually present with a cheek mass or swelling that is readily apparent and palpable clinically. Although many lesions have nonspecific characteristics on computed tomography (CT) and magnetic resonance imaging (MRI), there are conditions that do have distinctive findings. In general, the lack of specificity of imaging is inconsequential, as most lesions are excised, often for cosmetic reasons. This review is intended to enhance the readers' knowledge of the anatomy (Figure 1) and pathology of this often-overlooked space, thereby facilitating the diagnosis of lesions therein.
Anatomy
Figure 1 presents an overview of the anatomy of the buccal space and related spaces.
Borders
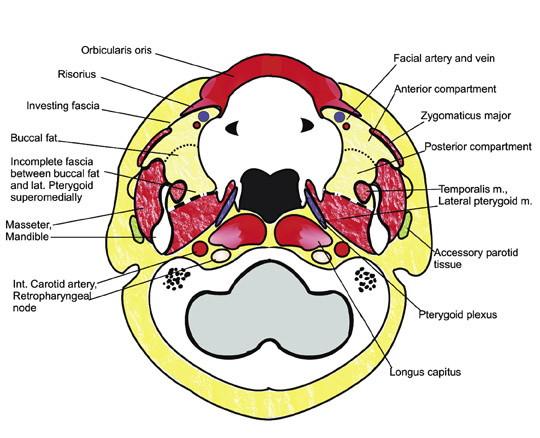
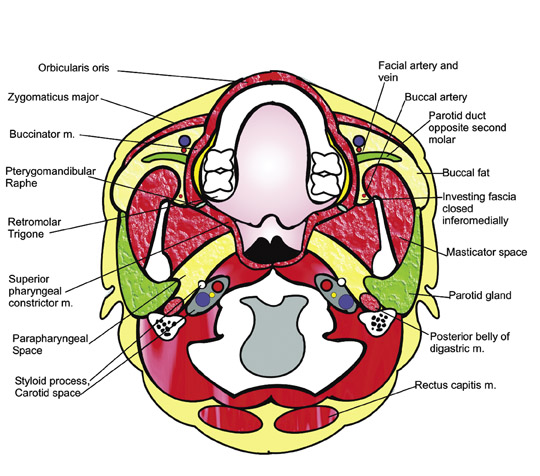
•Medial (Figure 1C)
a. Buccinator muscle
b. Pterygomandibular raphe-a fibrous band separating the oral cavity and the oropharynx that lies between the tonsillar pillar and the retromolar trigone. It may serve as a bridge for pathology to extend from the retromolar trigone to the buccal space.
•Anterolateral (Figure 1, B and C)
a. Orbicularis oris, risorius, zygomaticus major and minor muscles
b. Superficial layer of deep cervical fascia
•Posterior (Figure 1, B and C)
a. Masticator space
b. Parotid gland
c. Posteromedially, at the level of the hard palate (the superior aspect of the buccal space), the superficial layer of the deep cervical fascia (SLDCF) extending between the masseter and the buccinator muscle is incomplete, allowing spread of pathology between the buccal space and the masticator space. More inferiorly, this fascia is complete.
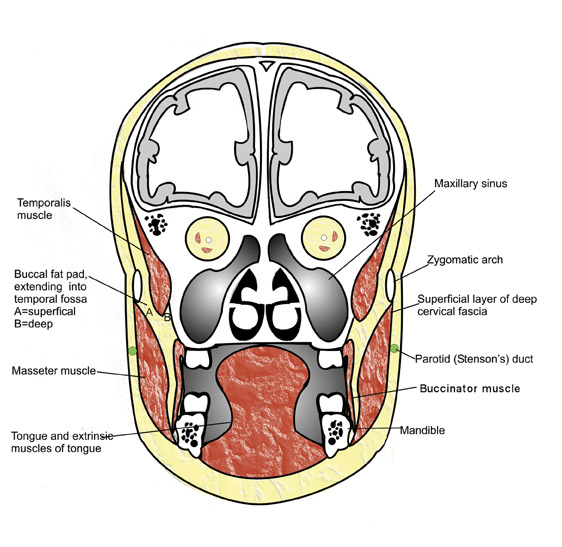
•Inferior (Figure 1, D and E)
a. Continuous with the submandibular space
•Superior (Figure 1, D and E)
a. Continuous with the temporal fossa
Contents
•Buccal fat pad
a. Anterior compartment-superficial to the parotid duct
b. Posterior compartment-deep to the parotid duct, contains specialized syssarcosis adipose tissue, a remnant of the succatory fat pad that aids in muscle motion and is of lower CT attenuation and of higher fat signal on MRI than all surrounding fat, including the anterior compartment.
c. Four extensions
i. Lateral--follows the parotid duct to the parotid gland
ii. Medial--between the mandible and the maxillary sinus
iii. Superior--further divided into deep and superficial based on relation to the temporalis muscle. The deep portion is adjacent to the lateral orbital wall, anteromedial to the temporal tendon. 4 The superficial portion is between the temporalis muscle and the SLDCF.
iv. Anterior--superficial to the parotid duct
•Parotid duct
a. Separates the buccal space into anterior and posterior compartments
b. Passes through the buccinator muscle at a level opposite the second molar, causing slight retraction of the mucusa and the submucosal fat
•Facial artery
a. Supplies the nasolabial region; direct branch of the external carotid artery
•Buccal artery
a. Supplies the posterior buccal space; branch of the maxillary artery
b.Enters space through the incomplete SLDCF posteromedially; anastomoses with the facial artery
•Facial vein
a. Located just anterior to the parotid duct along the buccinator muscle
b.Drains the nasolabial region to the external jugular vein via the deep facial vein. Infection may spread from the deep facial vein to the pterygoid plexus, to the inferior orbital vein, to the cavernous sinus.
•Nerves
a. Buccal branch of the facial nerve CN V (sensory to skin and the mucosa of the buccal space; originates just below the foramen ovale and enters space through the incomplete SLDCF medially)
b.Buccal branch of CN VII (motor to muscles of facial expression, originates within the parotid gland and courses parallel to the parotid duct)
•Lymphatic drainage
a. Buccal nodes to the submandibular nodes to the jugular chain
•Accessory parotid tissue
•Minor salivary (buccal) glands
a. Mucosa covering the inner surface of the buccinator muscle
Pathology may arise de novo within the buccal space and spread to surrounding structures or may arise in surrounding structures and spread to the buccal space. As discussed above, the lack of fascial compartmentalization superiorly, inferiorly, and posteriorly permits the spread of pathology. Other routes of spread include: 1) the pterygomandibular raphe and retromolar trigone and 2) the deep facial vein.
Pathology
Rhabdomyosarcoma
Rhabdomyosarcoma (RMS) is a malignant tumor of skeletal muscle. Approximately 40% of cases arise in the head and neck (orbits 36%, nasopharynx 15%, middle ear/mastoid 13%, sinonasal 8%, larynx 4%). 5 Rhabdomyosarcoma primarily affects children and young adults. It is the most common sarcoma in children and the seventh most common malignancy overall in children after leukemia, central nervous system tumors, lymphoma, neuroblastoma, Wilms' tumor, and bone cancer. Histological subtypes include embryonal/botryoid (75%, age <10), alveolar (20%, nodal metastasis are most common in ages 15 to 25), and pleomorphic (5%, poorest survival, ages 40 to 60). 5 Prognosis correlates more closely with extent of tumor than with histologic subtype. On imaging, skeletal muscle is invariably seen as the site of origin (Figure 2). MRI reveals a homogenous mass that is isointense to muscle on T1-weighted (T1W) images and hyperintense on T2-weighted (T2W) images (Figure 2B). CT shows a homogeneous mass that is isointense to muscle. The degree of enhancement is similar to that of the surrounding muscle (Figure 2A).
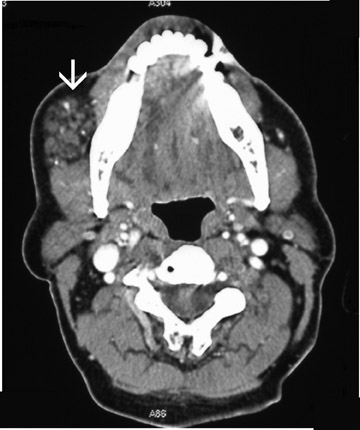
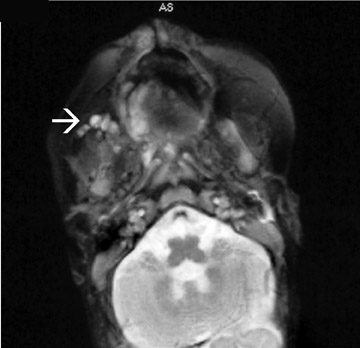
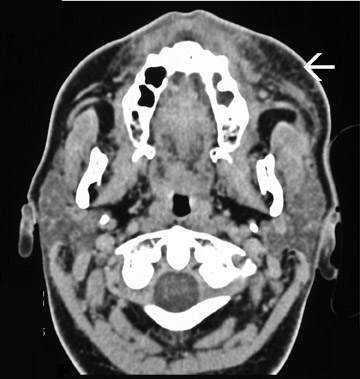
Congenital vascular malformation
There are 2 major types of vascular lesions, true hemangioma and vascular malformations. Vascular malformations are not neoplastic but congenital anomalies. They are further divided into capillary (port-wine stains or nevus flammeus), venous (cavernous), arterial (including arteriovenous malformation and ateriovenous fistula), and lymphatic malformations. Arterial malformations are considered high-flow lesions, whereas malformations lacking arterial components are low-flow. Vascular malformations are always present at birth but may not be clinically apparent until early infancy or childhood. They grow slowly and steadily but neither regress nor involute.
Skeletal changes are more common than with hemangioma, and vascular anomalies may be intraosseous or intramuscular. These lesions may undergo rapid enlargement with trauma, infection, or endocrine changes. Venous malformations are the subtype that most commonly affects the oral cavity. On CT, they enhance brightly and homogeneously and may contain phleboliths (Figure 3). Noncontrast CT shows a lesion of muscle density. With MRI, flow voids may be seen. The lesions are iso- to hyperintense to muscle on T1W images, hyperintense on T2W images, and readily enhance. Treatment is variable and includes steroid administration, laser photocoagulation, sclerotherapy, embolization, interferon administration, and surgical resection.
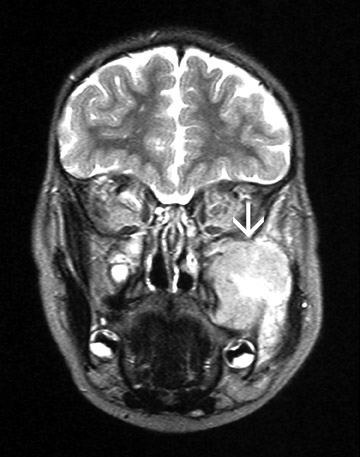
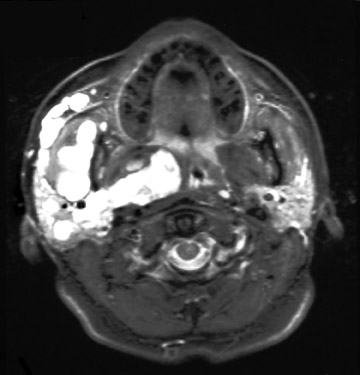
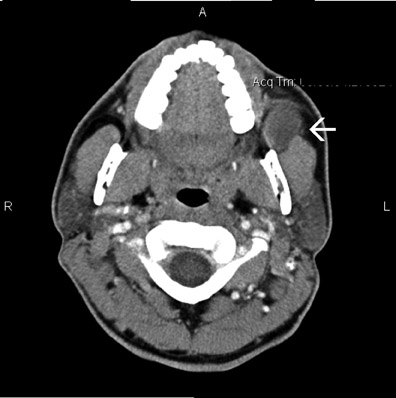
Infantile true hemangioma
This is a true neoplastic, benign condition. The term hemangioma should be applied only to lesions that present in early infancy, enlarge rapidly, and involute by adolescence. They are rarely present at birth, and 90% are evident by 6 months of age. Eighty percent are solitary, and there is a 4:1 female predominance. Fifty percent resolve completely by age 5; 70% resolve by age 7. 5 Clinically, hemangiomas are soft masses that may exhibit bruits and may change in size with crying or straining. During the proliferative phase, hemangiomas are high-flow lesions that may be confused angiographically with high-flow vascular malformations. CT and MRI findings are similar to those of congenital venous anomaly (Figure 4). Hemangiomas are usually untreated unless life-threatening complications occur. Such complications usually occur during rapid growth and carry mortality rates as high as 30%. They include include Kasabach-Merritt syndrome (consumption coagulopathy), airway compression, bleeding, and ulceration.
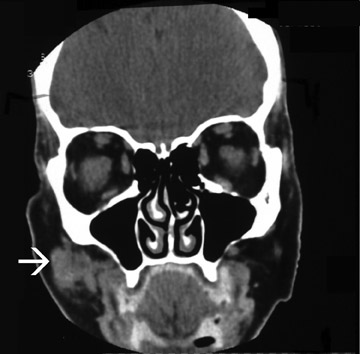
Cystic lymphangioma (congenital lymphatic malformation)
Lymphangiomas comprise 5.6% of benign lesions of childhood and infancy. 5 No race or sex predilection is observed. Although 90% are detected by age 2, 10% may present in adulthood (these are believed to be acquired posttraumatically). They are classified clinically and histologically into capillary lymphangioma, cavernous lymphangioma, cystic lyphangioma (hygroma), and lymphangioma-hemangioma. Capillary lymphangioma are cutaneous lesions that commonly affect the oral region. Cavernous lymphangioma are subcutaneous and commonly affect the oral cavity, neck, and tongue. They usually present within the first months of life. Cystic lymphangioma (hygroma) is most often present for imaging. Classically, it is seen to insinuate between adjacent structures and appear as cystic masses on CT and as high-intensity lesions on T2W images (Figure 5). There is a predilection for occurrence in the left posterior neck, but they are generally cervical. Complications may arise when mass effect is produced in places such as the submandibular and sublingual region, the tongue, and the floor of the mouth, causing dyspnea and dysphagia. This is especially seen in times of rapid growth secondary to trauma, hemorrhage, or infection. On imaging, they are large, single-or multiseptated masses of fluid density/intensity, which exhibit variable enhancement of the septae. Fluid-fluid levels may be seen with hemorrhage. High T1W signal may be seen with hemorrhage or lesions with high protein or lipid content.
Direct invasion by squamous cell carcinoma
Squamous cell carcinoma (SCCa) classically affects men aged 50 to 70 with a history of chronic alcohol and tobacco abuse. The behavior of SCCa in the oral cavity is different from its behavior in the oropharynx. The oropharyngeal mucosa, posterior to the circumvallate papillae, is endodermal in origin and is typically more affected by aggressive carcinomas, whereas the oral mucosa is ectodermal in derivation and is affected by less aggressive lesions. Oral SCCa tends to develop in 3 main areas: the floor of the mouth, the ventrolateral tongue, and the soft palate complex that includes the soft palate proper, retromolar trigone, and anterior tonsillar pillar. In any of these areas or in any of the structures around the buccal space, SCCa may invade directly. Lesions in the retromolar trigone may extend into the masticator or buccal space via the pterygomandibular raphe. 3 Squamous cell carcinoma has a variable, heterogeneous appearance on CT and MRI (Figure 6).
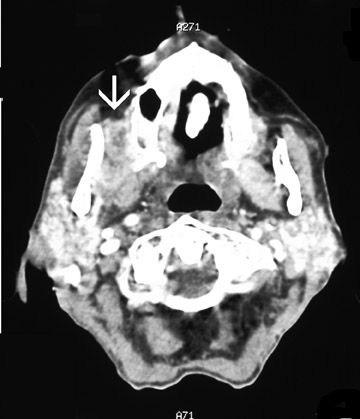
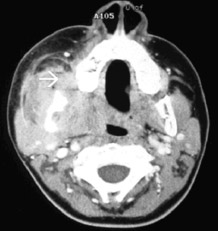
Cellulitis/abscess of the buccal space
Infection is usually secondary to dental infections or manipulation of calculi within the salivary gland duct system, including the parotid and submandibular gland ducts. Infection can arise de novo in the buccal space or can secondarily involve the space from surrounding structures and compartments, especially the masticator space and submandibular space, both of which have areas of free communication with the buccal space. Cellulitis of the buccal space occurs more often in patients <3 years of age, with females and males affected equally. It commonly occurs in fall/winter and may be associated with ipsilateral otitis media. CT and MRI show edema and swelling of the subcutaneous fat (Figure 7). Abscess may be seen in all ages. Diabetes mellitus and Crohn's disease are risk factors. Crohn's patients may have recurrent buccal space abscesses. 6 CT shows a hypodense mass with rim enhancement. T1W and T2W images show signal less than and greater than muscle, respectively, as well as rim enhancement.
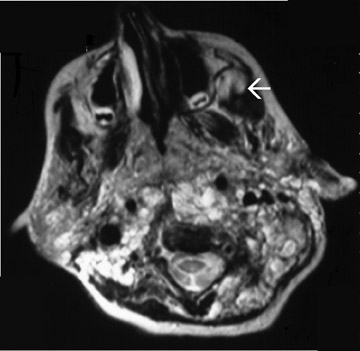
Schwannoma
Schwannoma is a nerve sheath tumor. While 13% occur in the extracranial head and neck, most are found in the lateral cervical region, where they originate from the sympathetic chain. The typical age of occurrence is 30 to 40, with a slight female predominance. On CT (Figure 8B), most of these tumors are of soft tissue density, homogeneous, and well-circumscribed, and most exhibit contrast enhancement. Cystic areas may be seen; they tend to be isointense to muscle on T1W images and hyperintense on T2W images (Figure 8A) and readily enhance.
Mucoepidermoid carcinoma
Any benign and malignant tumor of the salivary gland primordium may affect the buccal space. Pleomorphic adenoma is the most common. Other pathologies include adenoid cystic carcinoma, adenocarcinoma, acinic cell carcinoma, and basal cell adenoma. Mucoepidermoid carcinoma accounts for 2.8% to 15.5% of all salivary gland tumors 5 ; half of these occur in major salivary glands, half in minor salivary glands. In most series, it is the most common type of malignant mi-nor salivary gland tumor. The age of most common recurrence is 40 to 60, with a slight female predilection; however, any age may be affected. 5 These tumors exhibit different grades of behavior and, therefore, variable imaging characteristics (Figure 9). Previous radiation exposure may be a risk factor for development.
Liposarcoma
These tumors are rare in the extracranial head and neck but are common in the retroperitoneum and peripheral soft tissues. They have been reported in the cheek, lip, soft palate, floor of mouth, and submental regions. Their origin is from lipoblasts in or near surrounding fascia and not from pre-existing lipomas. They occur mostly in the fourth to sixth decades with a male predominance. Prognosis depends on histologic subtype. On CT, their density is greater than subcutaneous fat, and soft tissue elements are admixed (Figure 10). The mass is of lower density than muscle, however. On MRI, they exhibit fatty signal but of lower intensity than subcutaneous fat. Lipoma of the buccal space is much more common than liposarcoma.
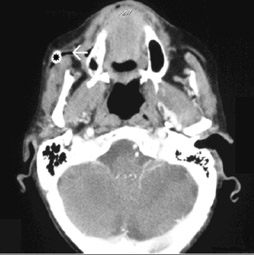
Plexiform neurofibroma, type I
Plexiform neurofibroma tumors are often seen in the subcutaneous tissue and extend without respect for fascial planes into multiple compartments. (The incidence of malignant transformation ranges from 3.1% to 15%. 7 ) Imaging findings show nodular and wormlike enhancement. Wormlike projections are seen along the nerve ends (Figure 11). This is pathognomonic of NF-I (Von Recklinghausen's disease).
B-cell lymphoma
Both Hodgkin's and non-Hodgkin's lymphoma (NHL) occur in the head and neck. Lymph node enlargement is the most common presentation. Non-Hodgkin's lymphoma frequently involves extranodal sites. Primary lymphoma of the salivary glands is rare and is classified as MALT (mucosa-associated lymphoid tissue) lymphoma, or MALToma. Imaging findings are nonspecific (Figure 12).
Granulocytic sarcoma (chloroma)
Granulocytic sarcoma is the tissue manifestation of myeloid leukemia and often precedes systemic relapse or progression from the chronic to acute blast form. The term chloroma comes from the green color of the immature myelocytes that are imparted by the enzyme myeloperoxidase in the cytoplasm. Imaging findings are nonspecific (Figure 13).
Ductolithiasis with sialadenitis
Most Stensen's duct stones are radio-opaque (Figure 14). Sialolithiasis is 8 times more common in the sublingual ducts.
Conclusion
The buccal space often receives less attention than the other spaces of the head and neck because of its small size and predominantly fatty composition. However, because of the close relationship to important structures both in and around this space, a variety of pathology may be seen. These structures include the parotid gland, masticator space, minor and ectopic salivary glands, lymph nodes, muscle, sinuses, facial artery and vein, and other neurovascular structures.